Dr Tejshri Shah, General Director of MSF and a paediatrician specialising in infectious diseases, recently returned from North Kivu, an eastern province of the Democratic Republic of Congo (DRC), the country at the epicentre of the current mpox epidemic in Africa.
In this short piece, she emphasizes that containing the virus in eastern sites for displaced people will be impossible unless efforts are made to listen to people’s needs and improve the appalling living conditions they have been struggling with for too long.
In Goma, many people I talked to seem to sense that something new, uncertain, and frightening is coming. But no one can predict what it will mean for them or how deeply it will impact their lives.

Mpox is not new in the DRC. The disease is endemic in several parts of the country, and notifications of cases have been on the rise for the past decade. However, in the Kivus, the virus has mutated into a form that seems to be more transmissible between humans, which is a significant concern as cases have been reported in very densely populated areas like Goma – a city of two million people – and in sites where hundreds of thousands have sought refuge due to the ongoing armed crisis in North Kivu.
While the lethality of this new strain remains limited, there is still reason to worry. Why? Because conditions necessary to prevent it from spreading in and around Goma are not in place, and the capacity to provide care for patients at risk of complications – young children and people with advanced HIV – remains limited.
Governmental and non-governmental actors must also urgently address the foundations of the mpox response, which must be adapted to the needs and realities of the people.Dr Tejshri Shah, General Director of MSF

How can we expect families living in tiny shelters without adequate water, sanitation facilities, or even soap to implement preventive measures? How can malnourished children have the strength to ward off complications? And how can we expect this variant – which is notably transmitted through sexual contact – to not spread in displacement sites, given the dramatic levels of sexual violence and exploitation affecting girls and women living there?
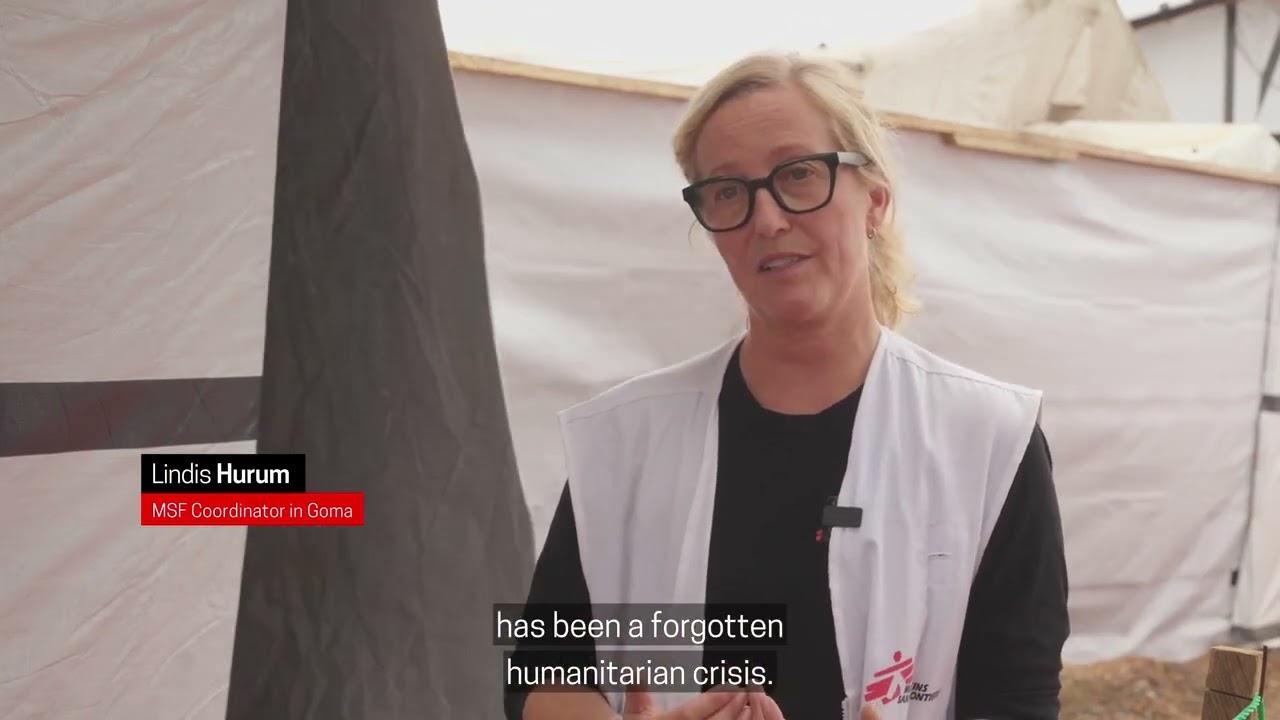
MSF has repeatedly denounced the inhumane living conditions that people face in the camps and the glaring gaps in the humanitarian response. More than two years after the start of the so-called “M-23 crisis” and the mass displacement it triggered, families living in the overcrowded camps still lack the essentials: food, water, safety, basic hygiene items, as well as access to sanitation and healthcare.
Mpox Cases Amidst Displacement Sites Near Goma
During a counselling session that I attended with survivors of rape, a woman told me she lives with her seven children under a plastic sheet. Her partner abandoned her after the rape. For women like her, the tried-and-tested solutions to prevent the spread of the epidemic are unimaginably challenging to implement. If she develops a rash due to mpox, she will be told to change her linens, wash everything thoroughly, disinfect her belongings, and isolate herself until she heals.
But how can she wash without soap and with only a few litres of water available each day? How can she isolate herself and protect her children while living together under their minuscule plastic sheeting shelter? If she isolates, who will get food for the kids? Who will collect firewood? Who will comfort the newborn?
For her and all those who have sought refuge in the displacement camps, the mpox epidemic feels like just another challenge amid a torrent of problems. Frankly speaking, it is not the most urgent one, given the daily struggles they face, including outbreaks of other life-threatening diseases such as measles or cholera.
Yet, mpox is there and needs to be tackled. To address this new, additional challenge, we need to make survival easier for people through a response tailored to their specific needs and real-life challenges. This starts by listening to people, understanding their needs and providing them with essential supplies for infection control: water, soap, disinfectant, and sanitary installations. These are simple but essential. We cannot rely solely on the arrival of vaccines to fix the problem. Improving people’s living conditions is also critical in fighting such outbreaks.

Together with health authorities, our teams do their best to provide care and raise awareness for those living on the sites, as we do in other parts of the country affected by the outbreak. Like many others, we hope that the long-awaited vaccines will arrive in the country as soon as possible. Yet, they will not be magic bullets: governmental and non-governmental actors must also urgently address the foundations of the mpox response, which must be adapted to the needs and realities of the people.













