South Africa has good TB policies, an impressive achievement that comes through in Step Up for TB 2020, a report released this week by Stop TB Partnership and Doctors Without Borders (MSF), which assesses TB policy in 37 high TB-burden countries.
For lives to be saved, though, the policy must be implemented, and when it comes to implementation of TB policy in South Africa there is much that still needs to happen in the area of TB implementation, which is a major leg of the World Health Organization's (WHO) strategy to "End TB" by 2035.
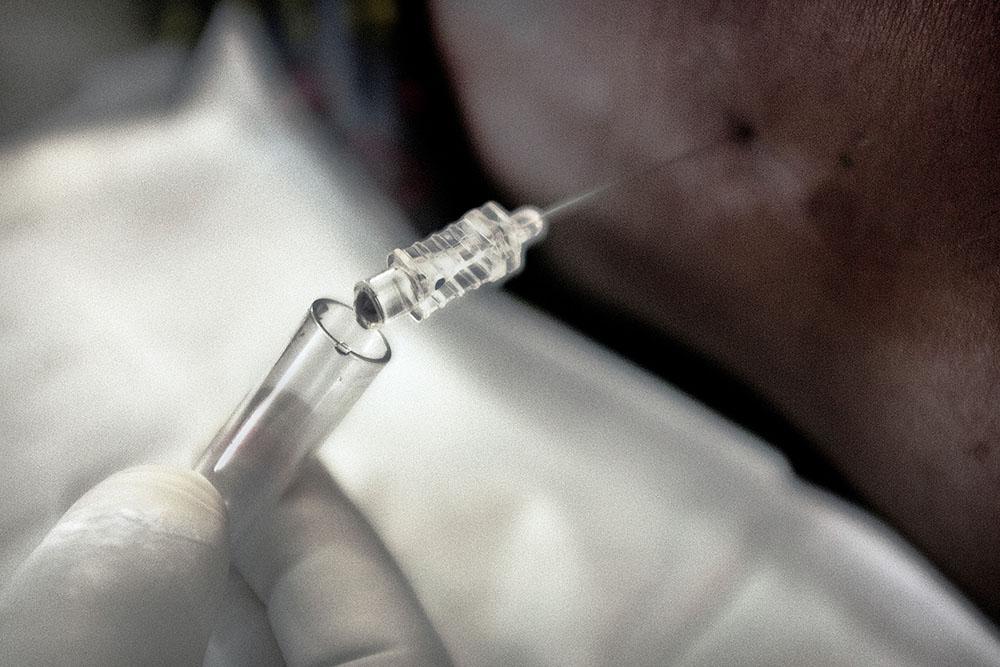
Preventative measures recommended by the WHO include active case finding, infection control, and timely treatment for people diagnosed with TB disease. The WHO also recommends that people with TB exposure who are at high risk of developing TB disease be offered TB preventative treatment (TPT)
Everybody Breathes: Part 1
Studies show the effectiveness of TPT in preventing TB disease ranges from 60% to 90% and protection can last many years.
At the United Nations High-Level Meeting (UNHLM) on TB in New York in 2018, world leaders committed to providing TPT to at least 30 million people by 2022, including giving TPT to 20 million people who live in the same house as individuals with clinically diagnosed TB disease. We are very far from reaching this target.
In the years since the UNHLM, only 6 million people have been initiated on TPT. To meet the 2022 target, the Stop TB Partnership estimates that over 6 million people who need to access the TPT in 2020 alone, something that is now thought impossible.
Why are we failing? The challenges are multi-faceted, but TB prevention programs piloted by MSF in Khayelitsha in the Western Cape and Eshowe in KwaZulu-Natal reveal some important implementation lessons.

In Khayelitsha, MSF launched a pilot program in 2017 that set out to screen for TB and follow up adolescents and children who had been exposed to drug-resistant TB (DR-TB) in their households, so that we would be able to respond quickly if these individuals did in fact develop DR-TB.
We chose to focus on older kids and adolescents because only 8% out of the estimated 25 000 children and adolescents who become sick with DR-TB each year are diagnosed and started on treatment.
Accessing this group was an extremely difficult task, and ultimately our program was only able to enrol 10% of eligible participants. We hit snags in both households and clinics. Perhaps the biggest stumbling block was the fact that we seldom found older children and adolescents at home – they tended to be at school, or out with friends. Those we did find generally needed to be accompanied to the clinic by their parent or guardian, requiring the parent or guardian to take a day off from work.

Everybody Breathes: Part 2
Few were willing to do this. Those who did agree to go to the clinic faced the additional barrier of long clinic queues, and clinic staff working under extreme pressure who prioritize curative services over preventative services like TPT.
In March, with South Africa in COVID-19 lockdown, we tried again, but this time our approach was home-based, with MSF teams conducting clinical assessments of the exposed children at their homes. We were also able to offer TPT this time around, made possible by the publication of new national guidelines in 2019 that significantly expand the eligibility criteria for TPT to include all DR-TB contacts considered to be at high risk of developing TB disease, including children and adolescents.
Earlier, to address barriers at the clinic level, we had identified specific TB champions – clinic doctors with a passion for TB treatment - who were more than happy that we refer individuals to them for TPT. The COVID-19 lockdown also meant that schools were shut and therefore a greater number of older children and adolescents were at home, as were their parents and guardians.

All of these factors contributed to the program being successful as a way to diagnose TB disease among household contacts, possibly preventing over 60 vulnerable individuals in Khayelitsha from becoming sick. The lockdown has now eased, and although children have not yet returned to school full-time, already the challenge of finding people at home has returned, underscoring the need for modified strategies to avoid the dissolution of this service.
In Eshowe, a mere 7 - 25 % of eligible adults received TPT between 2018-2020, while only 1 % of eligible children under the age of 5 have received TPT in 2020. The usual challenges are compounded by the realities of the rural setting, with many service users living among dramatic hills and deep valleys far away from their nearest health clinic.
Bringing TB testing and medication closer to patients
In 2019 we asked health care workers in Eshowe and Mbongolwane why they don’t prescribe TPT. They told us they were not certain what length of TPT regimens to give, as there is a perception that different guidelines advise different treatment durations. They also reported not always knowing which groups to target for TPT and that clinics often run out of Isoniazid, one of the antibiotics given to prevent TB.
However, recently enhanced efforts to find ‘missing’ TB cases provide an opportunity to improve the provision of TPT. Interventions launched by the Department of Health and MSF in Eshowe and Mbongolwane include the placement of TB screening officers at clinics, to increase screening and diagnosis of TB patients, and elicit contacts for all patients with a positive TB diagnosis.
Community-based teams then perform the contact tracing through home visits and if contacts are eligible for TPT, they can receive it at small community-based hubs for TB/HIV services.

These decentralized hubs save service users a great deal of travel expenses and queue time. MSF Eshowe also deploys TB ambassadors (volunteers who have previously been treated for TB or have family members who were diagnosed and treated for TB) to communities to conduct education on TB-related topics, including TPT. TB ambassadors are key in identifying patients that are potentially eligible for TPT, and they can also assist in ensuring they maintain treatment.
If TPT is to be successfully rolled out in Khayelitsha, Eshowe and other TB-affected communities, the health system needs to incorporate strategies that make TB prevention easier to access. This is possible by involving community health workers to offer services in communities and even homes or establishing after-hours services for groups who work or attend school.
Health promotion is also urgently needed to increase public awareness around TB and the importance of TB prevention, including TPT. Sadly, at present, TPT is not prioritized as an essential service in the health care system. To save more lives this needs to urgently change.