More than 1,000 people were admitted to hospital in a remote area of Democratic Republic of Congo (DRC) in 2015 after suffering toxic effects from ‘falsified’ or wrongly labelled drugs, says international medical organisation Doctors Without Borders (MSF) in an article published in The Lancet Global Health on 17th January 2017.
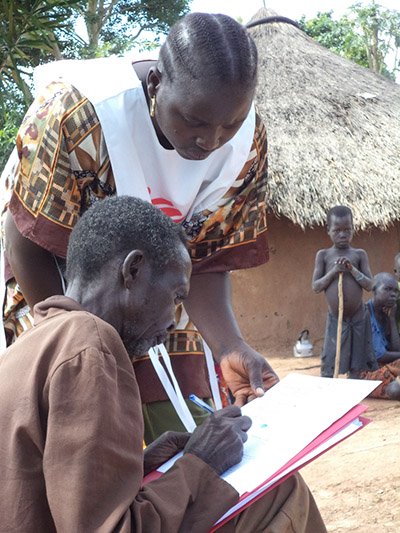
In late 2014, people began to arrive at health centres in Ituri district, near DRC’s border with Uganda, with symptoms including neck stiffness and involuntary muscle contractions. By August 2015, more than 1,000 patients had been admitted to health facilities run by MSF and the Ministry of Health.
Health staff initially suspected an outbreak of meningitis. However, further investigation suggested that symptoms were caused by patients ingesting a toxic substance. After analyzing samples of medications commonly prescribed in the area, the toxin was traced to tablets sold locally as the drug diazepam, but which actually contained haloperidol, an antipsychotic drug used in the treatment of schizophrenia.
Diazepam is generally used to treat a range of conditions, including anxiety and seizures, but in Ituri region, its use is even more widespread. Patients frequently receive diazepam to treat a wide range of illnesses, from sleeping disorders to headaches and even malaria,” says MSF’s Dr Nicolas Peyraud.
Haloperidol is known to cause acute dystonic reactions – or involuntary muscle contractions. “While these muscle contractions of the face, eyes, tongue, neck or arms are rarely life-threatening, they often cause distress, panic and shame for patients,” says Dr Peyraud.

MSF immediately alerted the Ministry of Health of DRC and the World Health Organization (WHO), which issued an alert identifying the suspect products.
An investigation is underway into how the wrongly labelled medicines came to be available on the market. The investigation is complex and is likely to involve drugs that have been intentionally falsified, and substandard medicines in general.
The existence of substandard medicines harms both individual patients and whole health systems. Weak regulatory systems for medicines, combined with inadequate penalties, corruption and porous borders, leave poor communities, in particular, extremely vulnerable to toxic and poor quality medicines.
“Poor quality medicines negate all the modern advances made in pharmacy and public health,” says Dr Peyraud. “This outbreak of severe toxicity through falsified medicines should be a wake-up call for the global public health community to ensure that all patients, especially those in vulnerable communities, benefit from well-advised prescribing and access to good quality medicines.”
More information on The Lancet Global Health