Tuberculosis (TB) remains the leading cause of death in South Africa, and yet it is curable. Why have we not overcome this fatal disease?
Doctors Without Borders (MSF) profiles five key strategies on which government and donors should focus their finances and efforts in order to end the deadly TB epidemic.
TB is curable, but there are numerous challenges that exist at every level of TB diagnosis and care - not only in South Africa, but around the world, where one person dies every 18 seconds from TB.
Five key barriers to effective TB treatment
- Toxic Treatment
- Unidentified TB cases
- Lack of social support
- Centralized drug-resistant TB (DR-TB) care
- Stigma
Barrier 1: Toxic Treatment
The past few years have several new drugs for treating drug-resistant tuberculosis (DR-TB). Yet there is still a long way to go— treatment is far from ideal, and only successful in half of all cases.
Multidrug-resistant TB (MDR-TB) still includes a painful daily injection of kanamycin that causes hearing loss in up to 60% of patients and can result in deafness.
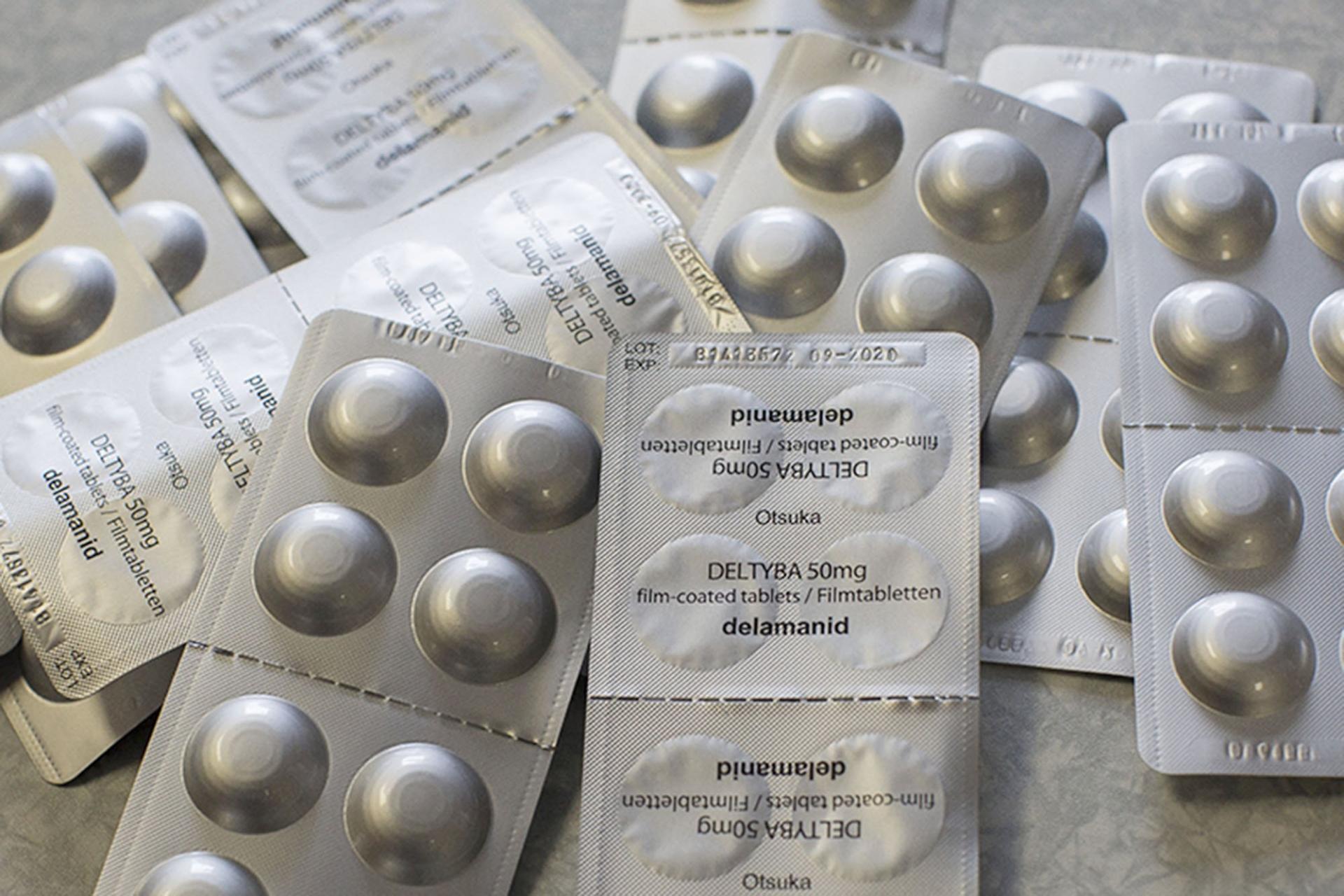
New drugs like bedaquiline and delamanid are becoming available to patients with more complex cases, but standard DR-TB patients may only receive these newer drugs after they have suffered irreparable harm from initial treatment—or may never access new drugs at all.
What kind of DR-TB treatment is needed?
“An ideal DR-TB treatment regimen would successfully cure a substantially higher proportion of DR-TB patients, have fewer side effects, and consist of only tablets—eliminating the need for a daily injection,” says Dr. Anja Reuter, a DR-TB doctor with Doctors Without Borders in Khayelitsha, South Africa.
Wider access to new drugs is central to this effort. “More research is needed to develop improved global DR-TB regimens, but steps can be taken now to give patients access to better treatment.
The World Health Organisation and governments should revise guidelines so that clinicians have the option to offer new drugs to people diagnosed with DR-TB, from the start of their treatment, as opposed to only after side effects have had a negative impact on patients’ quality of life,” says Reuter.
Barrier 2: Unidentified TB cases
In South Africa it is estimated there were 109 642 “missing TB cases” in 2016, meaning people with TB who have not been screened or diagnosed, and subsequently started on treatment.
This is concerning because TB left untreated leads to more suffering and death, and it drives transmission of the disease because TB is a droplet infection – everyone breathes, so anyone can catch it.
How do we find more TB cases?
According to Professor Kheertan Dheda of the University of Cape Town‘s Division of Pulmonology, “What is really needed to prevent drug-resistant TB (DR-TB) in the first place is we need to find the cases early.
By the time we make the diagnosis of DR-TB almost all the transmission has already occurred.” Preventing TB transmission requires greater investment in strategies for actively finding TB cases, and should be specifically targeted where the risk of TB is higher.
In South Africa, community health workers should be screening for TB as part of outreach health services in communities and at schools.
Targeted screening and diagnostic testing should be offered to populations at high risk of TB—such as those testing positive for HIV, those living in close proximity with known TB patients, and HIV-positive patients admitted into a hospital.
While South Africa has proactively scaled-up use in health facilities of GeneXpert—a TB test that returns diagnosis within two hours and detects whether a patient has drug-resistant TB—development of point-of-care diagnostic tools that can be used during outreach activities in communities is also necessary.
Barrier 3: Lack of social support
TB treatment is long, logistically challenging and can cause side-effects that make it difficult to lead a normal life.
Patient support is needed to help people cope and stay in care, yet this is lacking in most parts of South Africa.
Solution:
“Funding is needed to ensure the implementation of a quality counselling support package that includes treatment initiation counselling, a family home visit, contact tracing, and support when patients face problems,” says Leigh-Ann Snyman, DR-TB Patient support manager with MSF in Khayelitsha, South Africa.
Peer support forums are also essential. “My support group helped to keep me alive, it was where I was able to talk to someone who understood what I was going through,” says Goodman Mkhanda from Khayelitsha, who was recently declared cured of DR-TB.
Barrier 4: Centralized drug-resistant TB (DR-TB) care
In many parts of South Africa, the treatment of DR-TB remains centralized in hospitals, despite the fact that decentralization of DR-TB care has been the recommendation of the Department of Health since 2011.
Slow decentralization results in slower treatment initiation for patients—which means delays in reducing infectiousness and halting transmission of the disease.
Unlike HIV patients who have many options to collect their treatment close to home, TB patients lack choices. Long and costly journeys to overcrowded central hospitals, sometimes daily, cause many to simply give up on TB treatment.
“We would like to have decentralized as of yesterday, but we face infrastructure and resource challenges, and challenges retaining the nurses we train to manage DR-TB treatment at decentralised sites,” says Mduduzi Mbatha, District TB Manager with the KwaZulu-Natal Department of Health.
Solution:
Ultimately DR-TB treatment initiation and care need to be decentralized to primary health care facilities, with the most immediate urgency placed on high-burden districts.
Resources are needed to ensure that staff is adequately trained and that infrastructure and infection control measures are appropriate.
“My wish is that it [decentralization to primary health care facilities] can be fast-tracked, because it provides easy access to treatment for patients, and it also makes it easier for the clinicians working in these decentralized sites to monitor treatment and manage side effects immediately, so we minimize poor treatment adherence, and alleviate overcrowding in the treatment facilities,” says Dr.
Nempumelelo Khumalo, a DR-TB doctor at Catherine Booth Hospital in KwaZulu-Natal, South Africa.
Barrier 5: Stigma
TB is still highly stigmatised, being associated with poverty, social marginalisation, a risk of transmission and death.
In SA, 34% of respondents to a national stigma survey said they hadn’t shared their TB diagnosis to people outside their home; 36% reported being teased, insulted or sworn at because of their TB status. TB stigma is a major barrier to accessing care.
Solution:
Raising awareness about TB stigma, and educating communities is important for dispelling myths, and overcoming people’s fears around the disease.
In addition to official efforts, increased activism and consciousness from the TB community is needed.
“If patients and clinicians speak out about the challenges, in larger numbers, the barriers to effective TB care can be overcome,” says Dr Eric Goemaere, HIV TB coordinator for MSF.
Find out more about MSF's work in South Africa