

Eswatini (formerly Swaziland)
In 2024, Doctors Without Borders (MSF) opened a high-dependency unit (HDU) for patients requiring life support, and officially launched Sitsandziwe, a comprehensive sexual health clinic in Eswatini’s Manzini region.
The high-dependency unit is the first of its kind to operate in the Manzini region. High-dependency care had long been a health gap in Eswatini, with only three units operating nationwide. These are always full, potentially leading to premature deaths. The MSF HDU focuses on offering specialised care to critically ill patients, particularly those with non-communicable diseases, including cardiological and neurological conditions.
The unit currently has six beds and offers 24-hour care. We take referrals from all facilities in the area and discharge patients back to general wards, to a hospital with a higher or lower level of care, or to their homes, depending on their condition.
Featured
Our Activities in Eswatini in 2024
Data and information from the International Activity Report 2024.
90
9
€3.5 M
3.5M
2007
2007
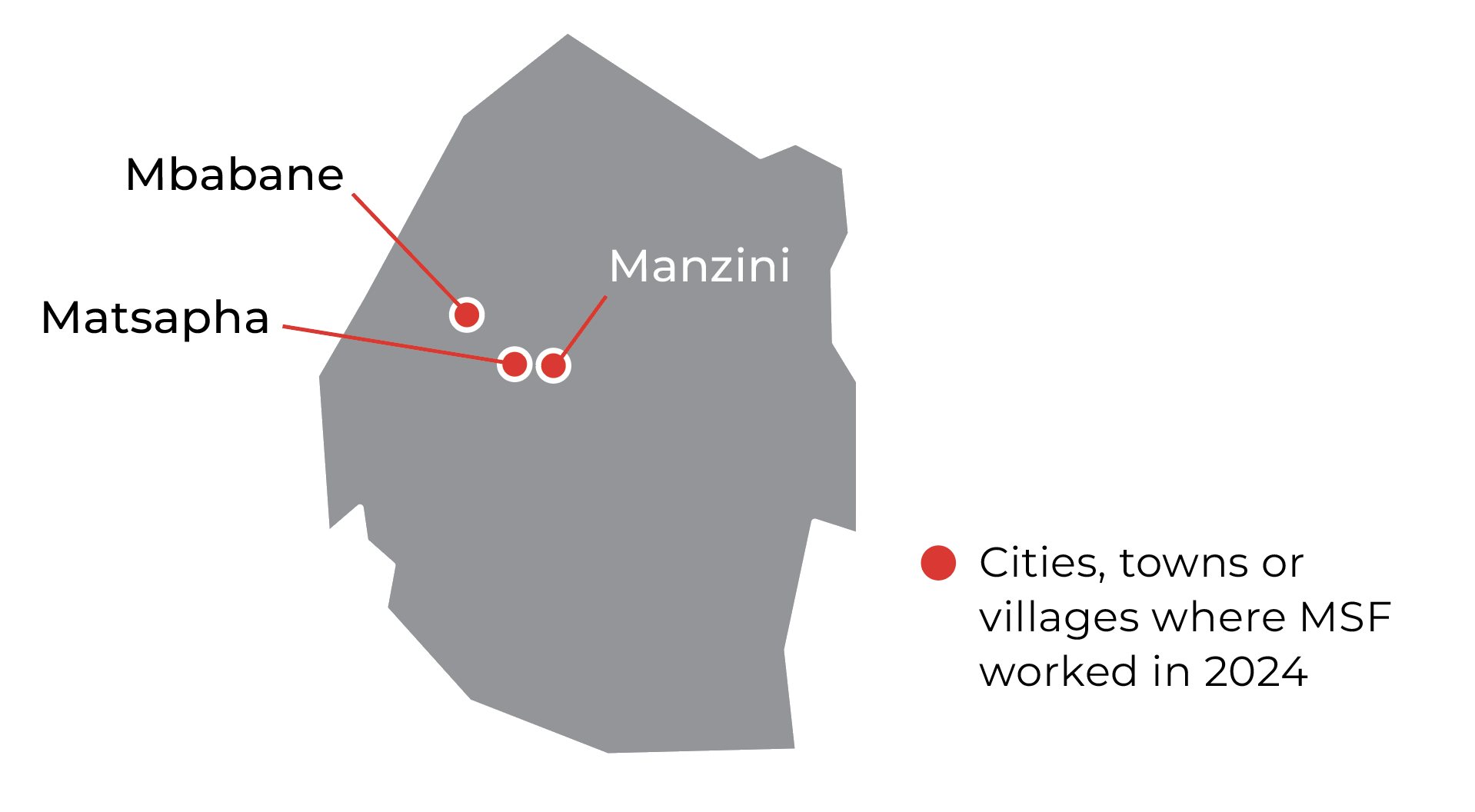
In the same project, we have a dedicated clinic for sexual and reproductive health in Matsapha Industrial Area, where we officially opened and run our Sitsandziwe clinic – which means ‘we are loved’ in English.
The clinic provides comprehensive sexual and reproductive healthcare, including family planning, laboratory-based diagnosis and treatment for sexually transmitted infections, screening for human papillomavirus, HIV testing and prevention, antiretroviral therapy for people living with HIV, and mental health support to marginalised communities.
Sitsandziwe addresses the diverse needs of the LGBTQI+ community, students, factory workers, and young women, implementing a patient-centred model of care and using innovative medical tools.
In 2024, MSF held four roundtables with community leaders, the Ministry of Health, MSF staff, and patients, emphasising our ‘People and Patients as Partners’ approach, where we made significant progress in informing and designing the care we provide. As a result, we have extended the clinic's opening hours to better meet patient needs, and strengthened our partnerships by supporting community outreach events.
In 2024

9,780
9,78
100
1
3,810
3,81


The End of the HIV Epidemic is Within Reach, Eswatini

MSF Prepares to Launch an Innovative Long-Acting HIV Prevention Program in Several African Countries

MSF Scientific Days 2024

MSF opens new comprehensive sexual health clinic in Matsapa, Eswatini

