Sex workers on the frontline of the HIV response in Malawi
*Names have been changed unless otherwise indicated*
Bernadette lost both parents when she was 7 years old and was taken in by her grandparents, who would send her to school without food.
“I started having sex in exchange for things as my grandparents were not able to provide me. This is how I got pregnant and dropped out of school,” says Bernadette who moved from her village to Dedza, Malawi at the end of 2018.
“When I became a sex worker I didn’t know anything about condoms, or any other family planning methods. I had heard of HIV but never thought about contracting it myself,” she says.
“This was the very first time I was given information on issues like HIV testing and sexual health,” says Bernadette after MSF community health worker Emily gave a health education session at the bar where she works and lives.
“I saw it as an amazing opportunity that could help me to be healthy, no matter my circumstances.” Emily listened closely to what she had to say, because she too was a sex worker, she knew where Bernadette came from and what she was facing every day.

In Malawi, where poverty and unemployment remain high, many women like Bernadette turn to sex work – offering sexual services in exchange for payment of some sort - to support themselves and their families.
Malawi has one of the world’s highest rates of HIV, and while the country has made huge strides in fighting the epidemic, sex workers remain extremely exposed.
With much lower access to health information and healthcare than their counterparts in the general population, sex workers are over five times more likely to contract HIV and face much higher risks of unwanted pregnancy and STI infections.

Sex workers report stigmatising attitudes and often violence in their daily lives – from police, clients, bar owners, and even partners. While these risks are seen by many as part of the job, empowering sex workers with knowledge and prevention methods is key to protecting their health.
“In the past, most sex workers shied away from visiting health centres for fear of discrimination and stigma especially if they were found HIV positive. If women needed post-exposure prophylaxis (PEP) [treatment that prevents HIV if taken within 72 hours of exposure], they just didn’t go to the hospital because they knew they wouldn’t be helped,” said Alice Matambo (real name), an MSF community health worker in Dedza.
"Sex workers need healthcare in their daily lives: if a condom bursts, if they have an STI, or need to be screened for cervical cancer.”

Recognising these gaps, MSF has been working with the Ministry of Health to provide services that meet the specific needs of sex workers.
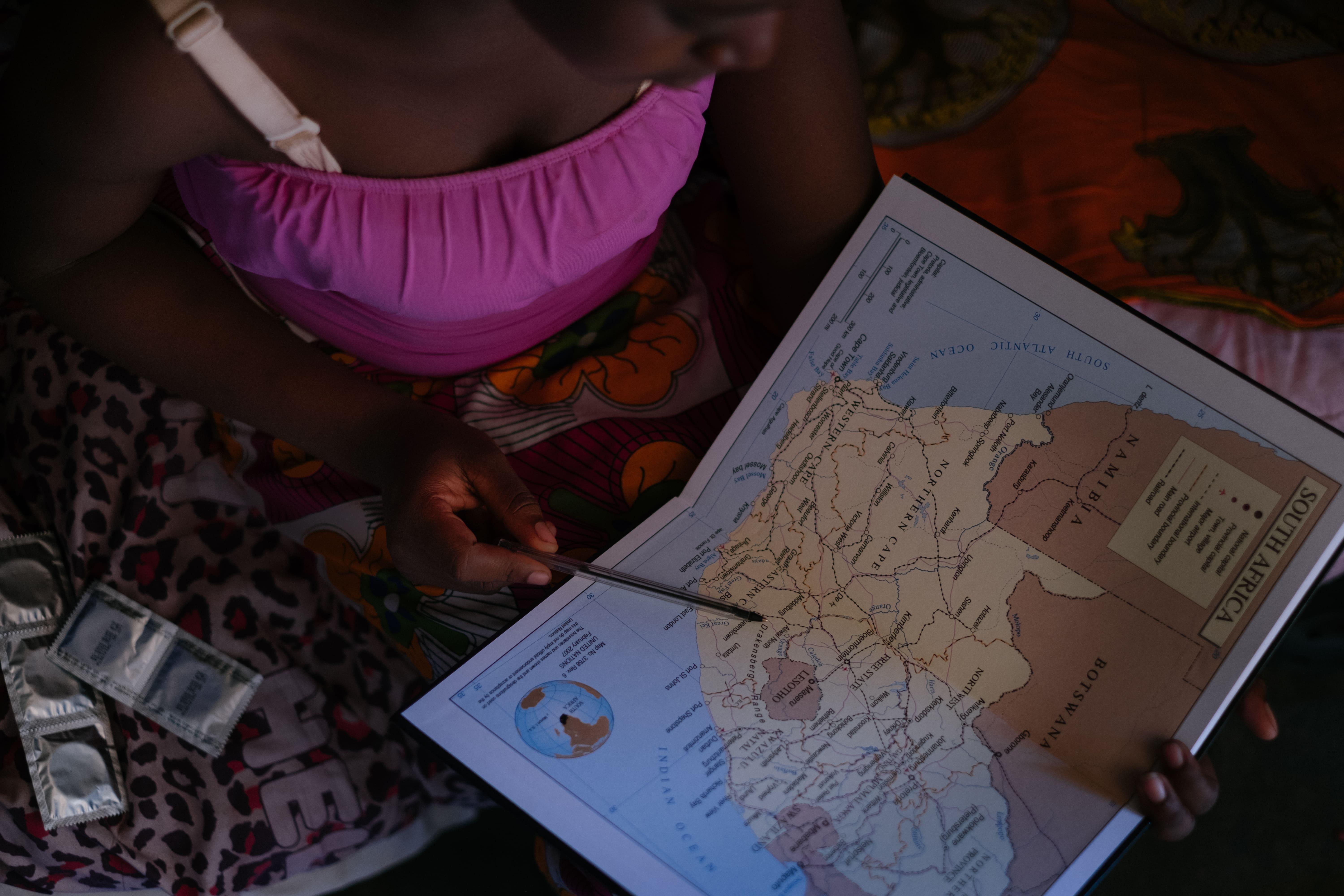
To connect with sex workers in the towns of Dedza, Mwanza, Zalewa, and Nsanje, MSF has trained sex workers like Emily and Alice as community health workers as they have themselves experienced the challenges and dangers associated with sex work.
This shared experience enables them to discreetly link with other sex workers, understand their health situation, and explain the medical services they need. Medical staff in the project have also been given sensitivity training to provide friendly services for sex workers.

“We approach sex workers gently and with respect, which makes them accept our approach, and look for medical help,” Emily says.
Margret, an MSF community health worker in Mwanza, explains this way of working. “My job includes going door to door and visiting bottle stores and brothels where I meet sex workers and provide them with information related to HIV testing and how they can take care of their health. For those who agree to be tested for HIV we set up a home visit,” she says.
The community health workers also guide sex workers towards ‘one-stop’ clinics run by MSF in the Ministry of Health facilities or in rented rooms in communities close to where sex workers live and work.

The ‘one-stop’ clinics are easy for sex workers to access discreetly and at convenient times.
In a single visit, clinicians provide services like HIV testing, treatment and counselling; TB screening and referral for care; and sexual and reproductive health care, including screening and treatment for STIs, access to choice contraception, cervical cancer screening, and treatment for sexual violence, which is either delivered on the spot or through referral.
“With these services, I feel more empowered than before and I am able to negotiate protection with the clients. I know how to put a condom on properly, and we now have lubricant which prevents accidents,” says Bernadette.
Many of the community health workers employed by MSF say they resorted to sex work after having children at a young age and being abandoned by their families or losing the support of their husbands to take care of their children.
They are often shunned by their families and communities, facing abuse and hostility because of what they do.
The presence of the program has seen reduced levels of stigma against sex workers in their areas, as well as a positive impact on their access to HIV testing and sexual health care.
“While some people used to look at us as animals, things have changed,” says Margaret.
“Today, the perception that people have towards sex workers is improved. Today, people understand that HIV affects everyone. And if we are to deal with HIV once and for all, the first step is to accept and recognize that, despite being different, we are all human beings.”

MSF Project
Since 2014, MSF has been working with national health ministries and partners to increase health care for sex workers and MSM (men who have sex with men)—people who often have a difficult time accessing health care—along main transport routes or busy centres of trade between Mozambique and Malawi through its ‘key populations’ project.
In Malawi, the project focuses on reaching female sex workers in Mwanza, Dedza, Nsanje districts, and in Zalewa in Neno district. All project sites combine outreach activities with a ‘one-stop’ clinic, located at Ministry of Health facilities or in the community, that address the specific needs of the sex workers like access to condoms and PEP (post-exposure prophylaxis), a drug which reduces the risk of HIV transmission.

In all sites, MSF employs sex workers as trained community health workers to reach their peers through discreet networks and community engagement.
By the end of 2018, 5,171 sex workers were enrolled in MSF’s project in Malawi and 1,797 were actively seeking regular care.
About half of the enrolled patients are HIV-positive of which 85% are virally suppressed, meaning that the women are able to take their treatment well, they are more likely to stay healthy and less likely to transmit the HIV virus in the event of unprotected sex.

Community services: Community healthcare workers conduct regular health education sessions in the community or in sex worker’s homes on topics including safer sex, HIV and STI prevention, sexual and gender-based violence, hygiene, family planning & contraception, and TB and cervical cancer.
They also provide sex workers with condoms, lubricant, emergency contraception methods, initial doses of PEP (post-exposure prophylaxis), pregnancy testing and screening for sexual violence.
On appointment, trained counsellors visit sex workers at home to provide HIV testing services, counselling, TB and STI screenings and referrals.

‘One-stop’ clinics: Trained clinicians offer a comprehensive package of HIV and sexual and reproductive care using a sex worker-friendly approach: HIV testing and initiation, counselling, refills of antiretrovirals, HIV care, and viral load monitoring, TB screening and referral, STI testing and treatment, family planning, care for victims of sexual violence, viral load, and cervical cancer screening and treatment.
The ‘one-stop’ clinics aim to address each sex worker’s health needs in a single visit.use the opportunity of each contact with a sex worker to address all of her health needs in a single visit.
Adeline, MSF community health worker, Nsanje
*not her real name
“One time a client raped me during a session. I never went to the police. I didn’t know about PEP [post-exposure prophylaxis, a drug which reduces risks of HIV infection after exposure] or that you can get treatment after being raped.
It was better to just keep quiet, so I did nothing. I’ve learned to take care of myself as a person and to live a healthy life. Having knowledge helps you to take care of yourself.”
Adeline became a sex worker in 2005, after divorcing her husband and being left with two children to support alone. She became a community health worker with MSF’s sex worker project in 2016.
Sex workers often experience violence and abuse from clients, police, and their partners, with cases, regularly reported to MSF teams.
Community health workers are trained to identify signs of sexual violence, provide psychological first aid and emergency contraceptives and link them to medical care if needed.
Rozi MSF community health worker
*not her real name
“Before MSF we couldn’t access health services the hospital. We were not looked at as individuals. When we went to the hospital with any ailment, we were told our illness was the result of the job that we chose.
Even if sex workers’ ARVs were finished, it was tough for them to go to the hospital for fear of insults from health workers, so they didn’t. This was putting the lives of many sex workers at risk of death.
“Everyone should be treated the same.
Care of the patients should be at the centre of the health ministry’s approach as well. If a sex worker is able to get health services, she is able to enjoy a healthy life free of diseases so she can do her work and support her family.”
Rozi* is an MSF community health worker with MSF’s sex worker project in Dedza, Malawi.
She became a sex worker in 2002 after a divorce left her with two children to support alone. Without any qualifications to find a decent job or capital to start a business, she chose to become a sex worker.
Each day she carries a backpack with HIV prevention materials, and flipcharts designed by sex workers on topics like HIV and STI prevention, sexual and gender-based violence, hygiene, family planning & contraception, and TB and cervical cancer.
Aisha* 18 years, young woman engaged in transactional sex, Mwanza
*not her real name
“When I was sixteen, I got pregnant. My parent advised me against abortion, they argued that I could die.
They offered to take care of the child. With the man that impregnated me not giving support, it was tough for me to care for my child. Due to the lack of ways to earn a living, I thought it was a good idea to start sex work.
The (MSF) community health workers advise us on how we should take care of ourselves to protect ourselves from contracting HIV, STIs as well as how to prevent HIV when we are forced into unprotected sex.
Aisha* 18 years, engages in sexual activities in Mwanza with clients in rented rooms in exchange for money.
In Malawi, the participation of females under 18 years in some form of sex work is considered as sexual exploitation and a contravention of human rights’ law. Yet many adolescents and young women in Malawi engage in some form of sex work in exchange for money or goods.
Ketisha*, adolescent engaged in transactional sex, 16 years, Mwanza
*not her real name
“To be honest, being a teenager playing my trade as a sex worker is not easy, especially with my age. I get asked why at my age I am at the bottle store instead of being at school.
They kind of take advantage of my age to say all sorts of things. My parents don’t know that I am a sex worker. For me to be a sex worker doesn’t mean I never tried alternative ways to support myself financially. I really tried.
When I look around, a lot of teen sex workers are facing a lot of challenges. They are being forced to sleep with older men without the use of any protection. If they protest, they are physically assaulted.
To me, MSF is my fountain of happiness. When the community health workers visit us, all they do is provide advice without looking down upon us. They are the most humble people you ever meet.”
Ketisha, 16 years, engages in transactional sex with clients in rented rooms in Mwanza. She was married and divorced at an early age after a man impregnated her.
MSF provides medical care to all women without distinction of age. Around 10% of those enrolled in MSF’s sex worker project in Malawi are under the age of 18, defined as sexually exploited adolescents.
These young girls are a particularly vulnerable group who face high risks of contracting HIV or STIs or falling pregnant.
MSF runs weekly sessions for at-risk adolescents with trained counsellors and health workers, where a comprehensive package of healthcare is provided, along with social activities and support from a social worker.
Jennifer* sex worker, Mwanza, 26 years
*not her real name
“My husband was a professional thief, and when I tried to talk him out of earning a living by theft the result was divorce. In the end, the only way I thought would help me support my two kids was to go into sex work.
When my relatives heard what I was doing, I was chased away. But blood is thicker than water, and later on, they welcomed me back.
I want to leave this business, it’s really tough. […] My most painful moment was being tricked by a client. Afterward, he refused to pay. To make things worse he didn’t use a condom. He just left.
By this time, I’d heard about PEP [post-exposure prophylaxis, a drug which reduces risks of HIV infection after exposure] from MSF so I ran to the hospital to get treatment.”
Jennifer* 26 years from Mwanza is a single mother of two children, became a sex worker in 2008. She receives a package of comprehensive HIV prevention and sexual and reproductive healthcare from MSF’s sex worker project in Mwanza.
In Mwanza, Zalewa, and Dedza, three transport hubs in western Malawi known, the presence of truck drivers, seasonal and industrial workers attracts a lot of sex workers.
MSF uses the ‘one-stop’ clinic approach combined with peer-led outreach services to reach sex workers who provide services for clients in rented rooms near transport hubs or at hotspots and bars.
Pictures by: Isabel Corthier