The media’s focus as COVID-19 has washed over the globe has largely concentrated on urban centers, a preoccupation that is justified by the high case numbers in cities. Yet, as the pandemic slows, it is increasingly clear that COVID-19 has not been a solely urban public health phenomenon. In September, photographer Chris Allen and writer Sean Christie documented the experiences, successes and lessons learned in the rural hinterland of South Africa’s KwaZulu-Natal province, where a community banded together to combat COVID-19.
“It is another reality in rural South Africa,” says Dr. Rosie Burton, an MSF infectious diseases specialist, who over the course of the epidemic has worked in district hospitals in three different provinces.
“What the epidemic has done in a place like rural KwaZulu-Natal is expose the horrendous inequity in the health system. At the same time, some really incredible initiatives have been established in rural areas,” she says.
Dr. Liesbet Ohler, Burton’s colleague, works in the KwaZulu-Natal town of Eshowe. She says that urban and rural settings have some challenges in common, like stigma, high levels of fear among health care workers, and issues around oxygen provision in hospitals, but that the differences exceed the commonalities.
“The distances between clinics are greater, there are fewer health resources and governance systems are often multi-layered, to name just a few of the challenges. Strategies that worked in cities are not necessarily a good fit,” she says.
Out of the box thinking is essential in under-resourced settings, as are strong partnerships at all levels of society, “because there is simply no way you will be ready to face such a fast-moving epidemic unless everyone pulls in the same direction,” according to Ohler.
Collaborating on Prevention
In the last week of March, with KwaZulu-Natal accounting for 16 of the 85 confirmed COVID-19 cases in South Africa and with people still travelling with little restriction, it was only a matter of time before COVID-19 entered uMlalazi sub-district in KwaZulu-Natal, where MSF has worked since 2011.
“We needed to implement prevention measures without delay,” says George Mapiye, MSF Deputy Field Coordinator.
To ensure that safe practices were widely embraced, MSF convened a diverse, multi-sectoral emergency response committee, which met weekly in the first months.
“Through this committee we saw to it that communities were educated and that a plan was put in place for pension payment days, when thousands of people flock to town. The Muslim community played a significant role by allowing the use of their public annoucnement system for the broadcasting of public health messages,” Mapiye says.
“MSF approached us to use our sound system, on which we give up the azzan (call to prayer). We were glad to assist, and through our own organisations we have been very active in securing and distributing food relief. Let's save lives, that’s the whole idea,” Deedat says.
Combatting stigma at health clinics
“In those early days we noted high levels of fear among health care workers in Eshowe and surrounding areas, as well as a general concern that visiting the clinic could increase a person’s risk of contracting COVID-19. It was important, therefore, to ensure that clinics had a strategy in place to separate COVID suspects from other clinic-goers,” says Ohler.
MSF assisted the department of health with establishing help desks outside clinics - triage points where all who wish to enter are screened using a screening tool, and possible COVID-19 patients are then referred to a separate tent for testing.

Sabelo Zulu, an employee of the community-based organization Shintsha Health Initiative (SHINE), a longtime MSF partner, says that the screening process outside local clinics depends on people being truthful about the way they feel.
He says that many people, fearing the stigma of being admitted to hospital for COVID-19, “might not answer screening questions truthfully.”
To counteract this, educators work the queue outside, sharing information and calming fears.
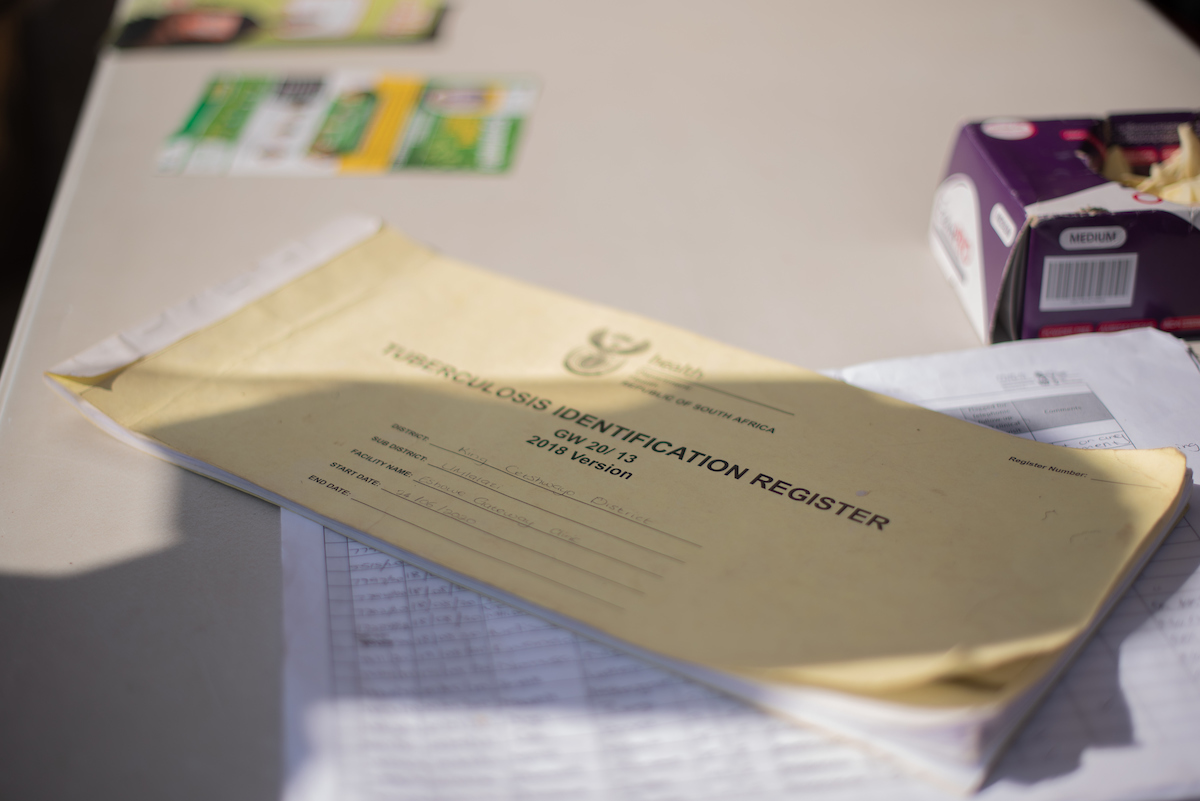
Zulu says that the decision to have the clinic’s tuberculosis (TB) officers staff the help desks was strategic.
“The symptoms for COVID-19 and TB are so similar, and if the person doing the screening doesn’t understand the subtle differences, there is a chance that TB symptoms will be mistaken for COVID-19, and people with TB will go undiagnosed,” he explains.
In normal times, clinic TB officers educate clinic goers on TB, provide screening services, collect sputum samples, conduct treatment initiation and enhanced adherence counseling and more.
Working with traditional leaders to reach communities
“There were so many rumours when this thing started, because people saw death on the TV. When they were told there would be testing, there were those older ones who thought that the government was coming to jova (inject) them with the disease, and they went to hide. In this place, people trust and listen to traditional leaders, and when they are sick many of our people first turn to a traditional healer,” says Bhekuyise Shandu, who is both an induna (traditonal leader) and inyanga (traditional healer) in the Mbongolwane area.
“When MSF first came to this place to deal with HIV they worked with us, using indunas to share information with the people and training traditional healers to pass information on HIV,” says Shandu. In May, he was trained by MSF and the municipality’s Environmental Health Unit on the government’s COVID-19 bereavement and burial guidelines, hygiene practices, anti-stigma messaging and more.
“COVID-19 has meant that we need to bury in a different way. Normally, the burial rituals happen over many days: animals are slaughtered, and many people come to pay their respects. Now, the coffin must go straight to the graveyard from the mortuary, and a maximum of 50 people can attend with social distancing,” Shandu says.
“Our people have accepted these changes and are observing them – we see to it,” he says.
Adapting care for patients at higher risk of infection
People living with chronic illness and compromised immune systems are at higher risk of dying of COVID-19, and South Africa is a country with approximately 7.7 million people living with HIV and an estimated 301,000 individuals with active TB. When COVID-19 hit, one of the biggest questions for the medical community was this: how do we protect people living with HIV and TB from the risk of infection in health facilities, while at the same time ensuring that vital health services for these vulnerable populations are maintained?
MSF in Eshowe came up with a strategy that aims to deliver medication for stable, asymptomatic patients with chronic conditions at easy-to-reach pick-up points in their communities.
“We worked out that there are approximately 19,000 individuals on anti-retroviral treatment in our area and designed a process for identifying which of these would be eligible to receive their medication at community pick-up points. 1,500 have been enrolled for this service to date, saving them time and money,” Ohler says.
When MSF took the decision to deliver chronic medication closer to peoples’ homes, it was the continuation of a program set in motion in 2019.
“MSF and the Department of Health had previously established 12 healthcare hubs in the rural communities, called Luyanda Sites. Luyanda means ‘Expand or increase’ in isiZulu, and the idea is to expand access to HIV and TB services for rural communities,” says MSF community program manager Neliziwe Mazibuko.
Luyanda Sites have served as convenient community pick-up points for chronic medications during the COVID-19 peak period, as they were all established with ease of access in mind, and it is additionally possible to keep medication at these sites for up to 2 days. An additional four permanent Luyanda Sites were opened in August, and 21 more pick-up points for chronic medication have been established in community sites such as schools, halls and churches.
“It is very ambitious - we worked until 10 or 11 at night in order to set this up - but it is a great thing, because, in as much as it was part of the COVID response, eligible people living in rural areas with HIV, TB and non-communicable diseases such as diabetes can now enroll for this service and continue to benefit from having their chronic medication delivered closer to home long after COVID has left us,” Mazibuko says.
Identifying and treating COVID-19 positive patients
Mbongolwane District Hospital was established by benedictine missionaries in 1937 and taken over by the Department of Health in 1978. Located atop a hill deep in rural Zululand and still framed by the twin towers of St. Joseph’s Church, this 200 bed hospital serves a population of roughly 70,000.
After positive cases were confirmed in the area in July, MSF worked with the hospital management team to set up an efficient patient flow system. This includes a “flu clinic” by the hospital gates, where patients exhibiting or claiming COVID-19 symptoms meet with a doctor.
“For most people who come to the hospital, the story ends outside the facility – they are seen and either triaged for a COVID-19 test or sent home with medication, and those who test are either asked to self-isolate at home or, if really sick, they are referred to the quarantine area, which is equipped to provide oxygen therapy,” says Dr. Helene Muller.
“The system works,” Muller continues, although she admits that, “working in full PPE inside the tents is a nightmare on hot days!”
While this system has worked to identify and separate COVID-19 patients, providing care for patients with severe symptoms has proven difficult in rural areas, says MSF nurse Buhle Nkomonde, who worked in the MSF COVID-19 Field Hospital in Khayelitsha, in Cape Town, before coming to Mbongolwane.
“In Khayelitsha, the district hospital was able to refer positive patients to a field hospital across the road, whereas all positives here are transferred to another hospital 70 kilometres away on bad roads. Ideally, we need to think of ways to capacitate rural district hospitals to treat COVID-19 patients on site, because we assume there's going to be cases at a much lower level for a longer time, and we don't know when the next pandemic will come,” Nkomonde says.
By 24 July, there had been 53, 604 confirmed COVID-19 cases in KwaZulu-Natal, a 420% leap in 20 days from the 12,757 cases reported for 4 July. In King Cetshwayo District, which encompasses Mbongolwane and Eshowe, case numbers rose 676% over the same period, from 531 to 3,591, with 48 recorded deaths from COVID-19. The District was lucky in the sense that COVID-19 case numbers peaked much earlier in many other parts of South Africa. Nevertheless, when the epidemic swept in, it initially sent the health system reeling, especially the secondary care institutions.
Senamile Ndlazi experienced firsthand the challenges of getting care for COVID-19 at this time. The young woman works in a grocery store in the town of Eshowe, and when a colleague tested positive for COVID-19 all of those who were contacts were told to report to the district hospital for testing.
“Nobody was available to test us at the time, and we were eventually tested at work. Most of us tested positive,” she says.
Ndlazi and her colleagues were quarantined in the hospital for at least 14 days.
“I had pains in my chest, but it seems there was little they could do for me - I just lay in bed for two weeks, receiving no treatment,” she says.
Her mother, Nondumiso Ndlela, says the experience was a frightening one for the whole family.
“After Senamile received her results nobody came out to screen or test the rest of the house, and we have elderly people and children living here. COVID came to Eshowe late, yet it seems that important parts of the local health system were still not properly prepared to deal with COVID-19 when it arrived. We can do better, and we must,” she says.
*
As COVID-19 case numbers dwindle in Mbongolwane and Eshowe, MSF has stopped most of the activities undertaken in support of the local response, and is once more turning back to its core obejctive, which is to tackle TB, a deadly respiratory pathogen which, like conrovarius, is spread via the air.
For Ohler and the MSF team in Eshowe, the COVID-19 epidemic demonstrated that previously unimaginable feats are possible when people and institutions work together.
“TB has been the world’s number on killer disease for years yet progress in addressing it has been slow, whereas in the space of half a year the world has developed point-of-care tests for COVID-19, multiple therapeutics, and we will likely have a vaccine in record time. Locally, the COVID-19 response drew together a record number of actors in a response which, while challenging at times, has left the local health system stronger, and more centred around the needs of patients,” says Ohler.
The support and donations in South Africa means that MSF is ready to offer care to patients in situations where healthcare isn't available.
All images by Chris Allan