An epidemic of hepatitis E is spreading through Burkina Faso. Between July 2020 and January 2021, MSF teams in the city of Barsalogho treated 730 people for yellow jaundice symptoms. Most were confirmed with having hepatitis E, a disease usually spread through contaminated drinking water. While symptoms are often mild, it is particularly dangerous for pregnant and breastfeeding women, causing complications and sometimes death.
Getting hold of clean drinking water is a major issue in Burkina Faso, especially for the more than one million people displaced from their homes by insecurity and scarce resources, says MSF epidemiologist Brama Diarra, who calls for a concerted effort to meet these communities’ needs.

What does the hepatitis E epidemic tell us about the humanitarian situation in Burkina Faso?
“The hepatitis E epidemic shows how difficult it is for people to get hold of clean drinking water. Our teams have identified various risk factors. These include a shortage of latrines, leading to people defecating in the open; a complete lack of the equipment needed to store and supply homes with drinking water; and a lack of soap, meaning people don’t wash their hands often enough. People also have limited access to medical care, so often resort to traditional medicine and obtaining medicines on the street.
The health hazards greatly increase in areas where displaced people live. There are too few water points, leading to a high population density around wells and other water sources. The water points are often unsanitary, encouraging the spread of parasitic infections and waterborne diseases such as hepatitis E, as well as cholera and various types of diarrhoea.
There is a lack of sanitation infrastructure and insufficient hygiene at all levels. Improving the living conditions of these communities, through better access to water, sanitation and hygiene, is therefore crucial. It is essential for preventing the spread of epidemics and waterborne diseases.

The situation in the city of Barsalogho is particularly severe. Very few people have adequate access to water, sanitation and hygiene facilities: just 34% have access to standard-quality water, 22% to safe and functional latrines and 35% have taken part in hygiene awareness and promotion programmes. Aid organisations need to organise themselves to tackle people’s immense unmet needs.
Other factors also increase the likelihood of epidemics, such as poor housing conditions. Many people live in overcrowded shelters in close proximity to domestic animals. Our teams monitor them closely for meningitis, measles, tuberculosis and COVID-19, depending on the season. We are also concerned that the dry and dusty Harmattan wind causes lung diseases, which can lead to more serious forms of COVID-19, increasing people’s risk of death.”

What is the biggest challenge in responding to an epidemic?
“The biggest challenge in responding to an epidemic is breaking the chains of transmission – ie preventing diseases spreading from ill to healthy people. We put in place preventive measures at three different levels. The first level involves measures to prevent people from getting ill in the first place.
These include vaccinations and any action aimed at reducing risk factors. The World Health Organization recommends vaccinating people in contexts such as this, to reduce the consequences of an epidemic on an already vulnerable population, but the hepatitis E vaccine is not yet validated by the country’s national health authorities and there is no large-scale production of the vaccine.

The second level involves screening and treating high-risk individuals and isolating and treating people who are sick, to prevent the illness from worsening or spreading to healthy people. Good communication is key in ensuring that communities support and comply to these measures. The third level involves preventing infected people from experiencing complications and relapses, which could lead to long-term effects, including permanent disability.
When tackling hepatitis E in Barsalogho, straight away we isolated the people who were infected, treated them and started screening the rest of the community. Community health workers referred more than 470 people to health centres, so reducing the transmission of the illness, at least a little. The people we treated as outpatients and at the health centre, as well as the wider communities, were given advice on hygiene measures and risk factors for hepatitis E.”
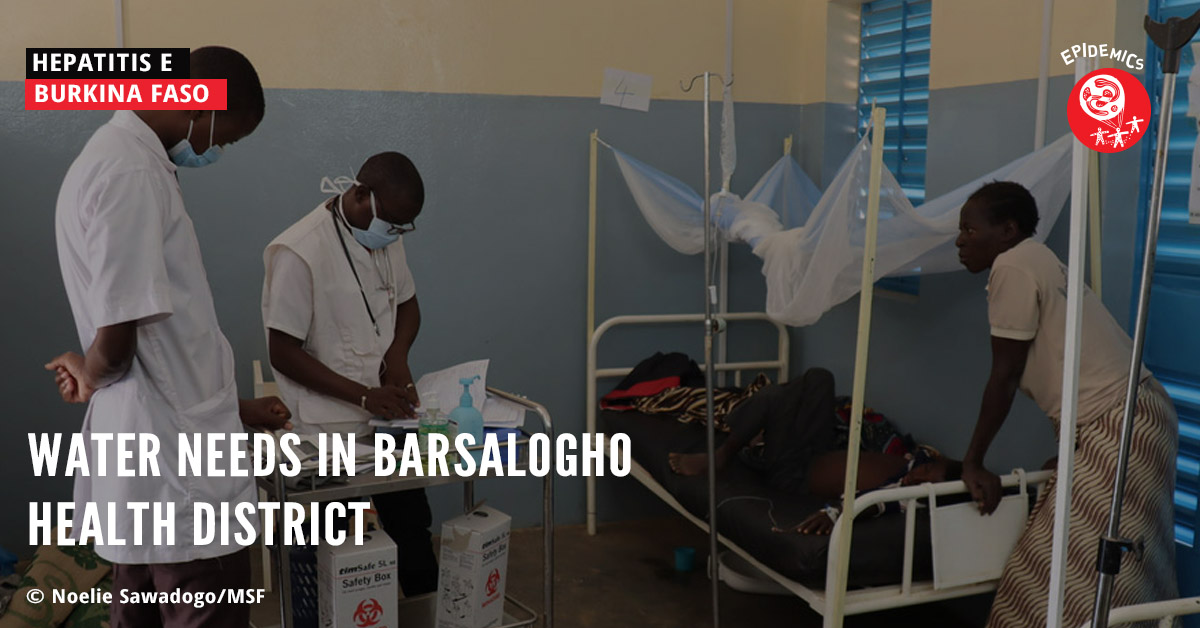
Play Video Water needs in Barsalogho health district
How can we reduce the risk of diseases spreading through communities?
“To reduce the risk of diseases spreading, we must promote good practices that help prevent infections as well as conduct disease surveillance activities. Improving disease surveillance mechanisms is also crucial, for example by strengthening community-based surveillance.
During this hepatitis E epidemic, we’ve organised awareness programmes for the communities and worked to improve their access to clean water. We’ve distributed kits containing soap, jerrycans to store water and water purification tablets for household use, because water quality directly impacts people’s health. We’ve also worked with other organisations in the region to collect and sanitise dirty jerrycans. Our teams have also constructed latrines in sites for displaced people.
Yet despite these concerted efforts by several organisations, a lot of work remains to be done to meet the needs of the communities in Barsalogho and elsewhere when it comes to water and sanitation. MSF is foremost a medical organisation, so other organisations must step up to help. Long-term investment in water, sanitation and hygiene activities, as well as coordination between specialist organisations on the ground, are essential for eradicating waterborne diseases, which are one of the leading causes of diseases for which MSF treats people every year.”



