On June 16 from 14:00-17:00 CET, the World Health Organization (WHO) will host a virtual “call to action” on the need to scale up access to preventive treatment for TB, led by WHO Director General, Dr. Tedros Adhanom Ghebreyesus. At the event, there will be a round-table discussion on the importance of investing in TB prevention, where implementing countries and partners will share experience from the field. Because of her innovative work with the MSF DR-TB Post-Exposure Program in Khayelitsha, South Africa, Sister Ivy Apolisi will be featured as the ”Voice from the Field” to inspire other countries to improve access to TB Preventive Therapy (TPT). Below is a summary of the remarks she will share.s.
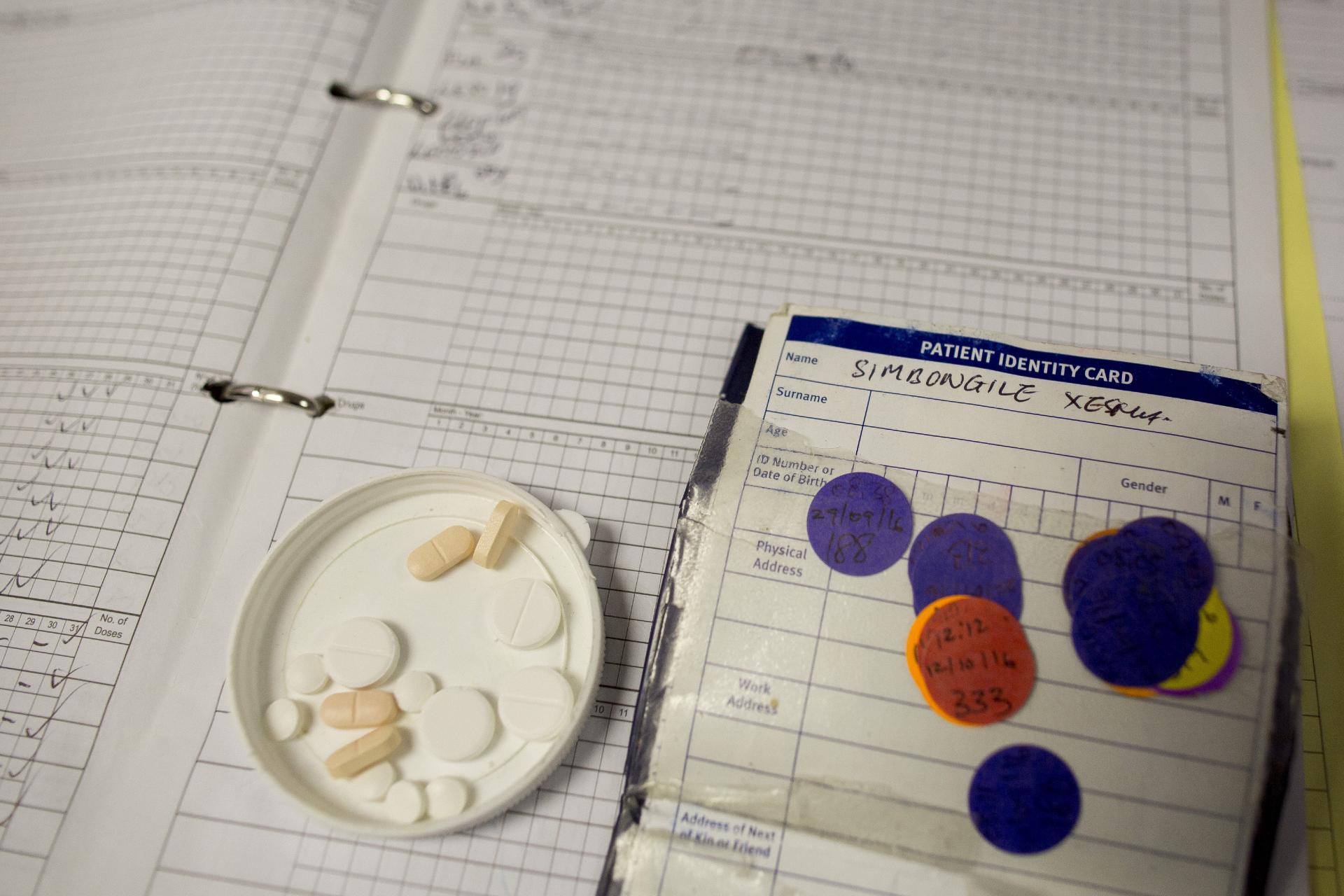
My name is Sister Ivy Apolisi and I am a nurse working with the humanitarian organization Doctors Without Borders (MSF) in our project in Khayelitsha. Since 2018, I have led our post-exposure program (what we call “the PEP”) for children and adolescents who have been exposed to drug-resistant tuberculosis (DR-TB) within their households. Drug-resistant TB is a serious problem in Khayelitsha—a community of more than half a million people located outside of Cape Town, South Africa that has a high burden of HIV, TB, and DR-TB—and there have only been limited interventions aimed at TB prevention. Our team has been supporting community-based DR-TB work in Khayelitsha in partnership with the city, provincial and national departments of health since 2010, and when we saw family after family being ravaged by the disease, we realized we had to get more involved in efforts to prevent what seemed like a never-ending cycle of DR-TB.

When we started in 2018, almost nobody was focused on what to do for older children or adolescents who were exposed to DR-TB, since most TB preventive efforts were focused only on children who were either living with HIV or who were under the age of five years. So we planned and began implementing a program where we would offer screening services to older children and adolescents who had a household member who had been diagnosed with DR-TB. We would request them to come to the clinics, ask them about symptoms, and offer those who were symptomatic chest X-rays and sputum testing. Even though DR-TB is a big problem in our community, we were only able to enroll about 39 household contacts in the program in two years.
When COVID-19 hit in 2020—and Khayelitsha was an initial COVID-19 hotspot in South Africa—we had to drastically change the way we did things! We began offering home-based care to people living with DR-TB to shield them and their family members from possible COVID-19 exposures at health facilities. This included doing home visits and assessing household contacts out in the community. These COVID-19 related changes also coincided with an update to the South African national DR-TB guidelines that allowed us to offer preventive therapy to high-risk household contacts who were exposed to DR-TB in the home. Given the worsening poverty and food/economic insecurity caused by COVID-19, most of our household contacts were living in very high-risk situations. So we were able to adapt out PEP to offer not only screening but also preventive therapy for DR-TB. Although overall health services struggled during the time of COVID-19, the PEP actually took off in many ways. We were able to enroll more than 100 household contacts in just over 12 months.
We must all dedicate ourselves to stopping the ongoing cycles of suffering that seem to occur in families affected by DR-TB, and we hope that by sharing our experiences from Khayelitsha, we can inspire others to undertake similar efforts to end TBSister Ivy Apolisi

We were able to enroll more than 100 household contacts in just over 12 months. We learned many important lessons along the way that we think are important to share with others, including:
- Community-based treatment where screening and services are offered at a household level are likely to be much more successful than those based at the clinics. Such services really allow the health care team to actually see what is going on in the home, who is staying there, and the kind of challenges the families with DR-TB face that need to be addressed;
- Programs that offer preventive treatment and not just active screening may be more acceptable to families, especially in the time of COVID-19 when they are really worried about lung health. Most of the children tolerated DR-TB preventive treatment well, with more than 85% of our cohort completing six months of therapy—a finding likely facilitated by the use of preventive monotherapy coupled with counseling and psychosocial support. Preventing DR-TB in children and adolescents was so much better than watching and waiting to see if they got sick!
- Using a family-centered, non-judgmental, child-friendly approach likely contributed to the success of our PEP project, as families were supported to share their DR-TB status and have their children screened. Our pediatric DR-TB disease case detection rate doubled as part of the program (and children with DR-TB disease found through the PEP program had milder disease that could be treated in the community) and children were offered child-friendly formulations of the medications they needed for prevention and treatment;
- Most of the work can be done by nurses with telephonic support and home visits, especially if multi-month refills of preventive therapy are provided: collaboration between the department of health and the various stakeholders in the community strengthened our PEP collaborative approach

Much work needs to be done to improve access to TB preventive therapy for household contacts of all ages, including those exposed to DR-TB. What we found in Khayelitsha was that moving beyond the usual target populations was not only important—given that COVID-19 likely increased household transmission of DR-TB—but also doable if the care was provided by a nurse-led, multi-disciplinary team based in the community and working at the household level. Our program was able to build trust, and families reported that they felt cared for by the services we offered to them, which took into account their needs and the barriers they faced. We must all dedicate ourselves to stopping the ongoing cycles of suffering that seem to occur in families affected by DR-TB, and we hope that by sharing our experiences from Khayelitsha, we can inspire others to undertake similar efforts to end TB. We urgently need funding and political commitment to support these life-saving efforts.