MSF highlights again the urgent concrete actions that should be taken to turn a corner on this pandemic. Mistakes from the COVID-19 response must not be repeated in future pandemic planning.
“The global response to the pandemic has failed to deliver equal and equitable access to date, with the world now divided into a limited number of countries where people can protect themselves from this killer disease, and the majority of countries where people are left vulnerable to it. The longer the world is divided into COVID-19 haves and have-nots, the longer the pandemic will drag on, the more variants can develop, and the more deaths and suffering will occur. It is not too late to turn the corner and course correct so that the world can finally get ahead of the wave with this pandemic.
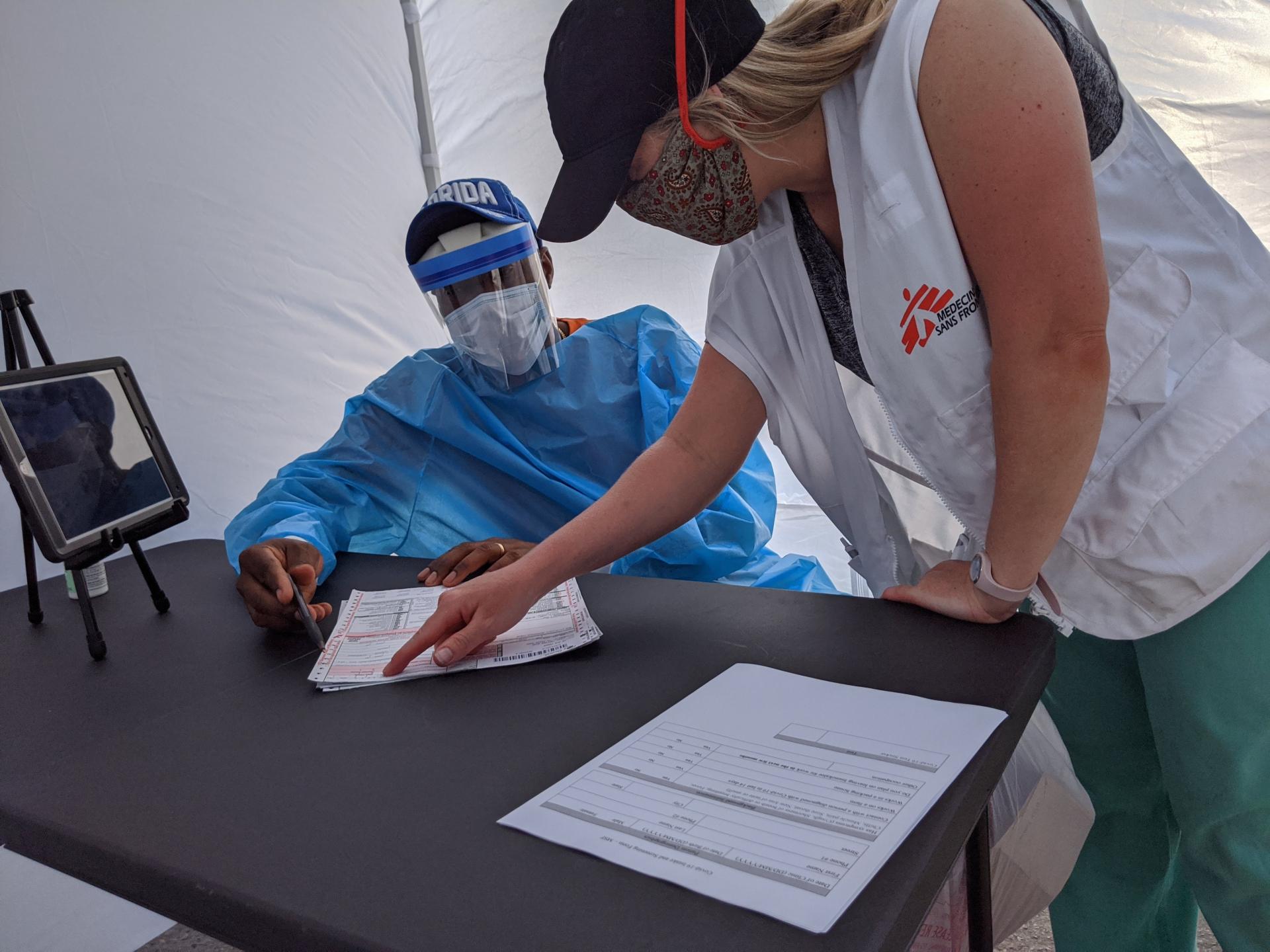
“In places where MSF works, we have witnessed the near-collapse of health systems under the burden of a disease which is now largely preventable. The dramatic lack of access to vaccines, treatments and diagnostics in countries in Africa, Asia and Latin America is both devastating and unconscionable. The prolonged inequity and overarching socio-economic impact of the pandemic risks further deteriorating access to healthcare in many low- and middle-income countries.

“As the world heads toward five million lives lost to COVID-19, high-income governments need to urgently do three things so we can turn a corner on this pandemic:
- Immediately redistribute their excess COVID-19 vaccines well before these doses expire to low- and middle-income countries that continue to dramatically lag behind in vaccination coverage via COVAX or regional procurement bodies, and make sure these countries are supported for vaccine rollout;
- They must use all their power to compel pharmaceutical corporations to share mRNA technology and know-how with the World Health Organization’s COVID-19 mRNA Vaccine Technology Transfer Hub in South Africa, and
- Share technology and know-how to produce monoclonal antibody treatments; and all governments must get behind the TRIPS Waiver supported by more than 100 countries at the World Trade Organization, which will allow all governments to remove intellectual property barriers and increase supply and availability of COVID-19 treatments, diagnostics and vaccines during the pandemic so that many more lives can be saved.
“Based on our experience in resource-limited settings, we know governments must prioritise funding not just for delivery but also strong health promotion and dialogue with communities to counter disinformation and fear resulting in vaccine hesitancy. We also urgently need to reach people ‘outside’ the system – refugees, internally displaced persons, migrants, and those living in non-government-controlled areas.

“An important barrier that must be overcome is the legal liability question that has hampered truly reaching the most vulnerable, wherever they are in the system. As vaccines receive full authorization for use, this should be followed immediately by pharmaceutical companies resuming liability responsibility for their own products. Continued acceptance of this transfer of responsibility and talks of waivers only serves to normalize a set-up that should not have existed in the first place.
“It is time to look critically at the root causes of the access crisis in this pandemic: the structural inequality in the global health system which concentrates decision-making power and ownership of lifesaving health technologies in the hands of a few powerful nations and their pharmaceutical corporations. Any mechanism to improve the current pandemic response and future pandemic preparedness and response should not repeat the mistakes made during COVID-19 to date and be firmly rooted in multilateral cooperation with clear accountability for high-income governments and pharmaceutical corporations in particular.
“Every day that goes by, another roughly 10,000 people are lost to this disease – what are governments with the power to change this horrific statistic waiting for?” says Dr Maria Guevara, MSF International Medical Secretary.
As countries convene to discuss the pandemic response at the United Nations General Assembly this week, Doctors Without Borders (MSF) calls on governments to urgently resolve the glaring inequity in access to lifesaving COVID-19 medical tools for people in low- and middle-income countries (LMICs).
Throughout this year, MSF has addressed critical needs and experienced struggles in providing care for people facing COVID-19, in countries ranging from India, Lebanon and Yemen, to Brazil, Mexico, and Peru. To date, more than 4.5 million people have died of COVID-19 – the pandemic is still a daily life-or-death emergency for millions of people around the world.
We urge all countries act in solidarity and support following measures to ensure that each country has sufficient tools to save as many lives as possible in this pandemic:
Today global vaccine inequity is severe, and people are dying. We have witnessed the massive stockpiling of vaccine doses by some high-income countries as the rest of the world goes without. The world now faces a situation in which healthcare workers and high-risk populations in LMICs may not receive their first doses until after the majority of high-income countries are fully vaccinated.
The fastest way to save lives right now is for high-income countries – including the US, UK, Canada, and Germany – to immediately redistribute their excess vaccine doses to LMICs, via the COVAX Facility and other regional mechanisms. This must be done well before these doses expire. MSF urges countries that have already vaccinated their vulnerable populations to stop purchasing additional doses and redistribute excess doses to support World Health Organization (WHO) targets of vaccinating at least 40% of all people globally by the end of 2021 and 70% by mid-202
Based on our experience in resource-limited settings, governments must prioritise funding not just for delivery but also for strong health promotion and dialogue with communities to counter disinformation and fear resulting in vaccine hesitancy. We also urgently need to reach people ‘outside’ the system – refugees, internally displaced persons (IDPs), migrants, and those living in non-government-controlled areas.
As the pandemic remains out of control and with the emergence of new and more transmissible variants, the need to dramatically increase the global production and supply of vaccines is obvious. Vaccine manufacturing capacity must be boosted in LMICs by utilising all policy and legal measures, including through full transfer of mRNA vaccine technology and know-how by the pharmaceutical corporations Pfizer (US), BioNTech (Germany), and Moderna (US). To dramatically boost vaccine supply in LMICs, and attain independent sustainability, full transfer of such technology needs to happen transparently and be open to all competent alternative manufacturers.
High-income countries, particularly Germany and the US, which host BioNTech, Pfizer and Moderna, should demand these companies share their mRNA vaccine technology and know-how with the WHO COVID-19 mRNA Vaccine Technology Transfer Hub based in South Africa. High-income countries should also provide financial and technical support to the Hub.
In addition to vaccines, the world urgently needs access to newer therapeutics and diagnostics to reduce the number of hospitalisations and deaths in this pandemic. The slower and lower rate of vaccination in LMICs increases the risk of transmission and variant spread, locally and globally.
In the face of ongoing and new waves of the virus around the world, health systems are being pushed to their limits, highlighting the urgent need for diagnosis and treatment of people with COVID-19. Yet, new WHO-recommended COVID-19 therapeutics, such as tocilizumab (produced by Roche, based in Switzerland) and sarilumab (Regeneron, US), remain out of reach for people in LMICs due to high prices, limited supply, intellectual property (IP) barriers, and absence of transparent access plans.
MSF calls on all governments to take actions to overcome the market monopolies held by the pharmaceutical companies, and support biosimilar production to lower prices and ensure sustainable access to these important new therapeutics.
Further, countries must support the ‘TRIPS Waiver’ proposal at the World Trade Organization (WTO), which if adopted would provide all countries with an expeditious way to remove key Intellectual Property (IP) barriers and legal risks around production and supply of COVID-19 medical tools, including vaccines, treatments and diagnostics, during the pandemic. Nearly a year after the Waiver was first proposed by India and South Africa; it is now supported by over 100 nations, while a small group of high-income countries continues to oppose it. These countries – particularly the European Union (EU), UK, Switzerland, and Norway – must stop blocking this lifesaving pandemic initiative supported by a majority of the world.
Countries should collectively acknowledge the limitations of relying on the pharmaceutical industry’s ‘good will’ to stem a global pandemic, and instead, support the will of LMICs demanding self-reliance through the TRIPS Waiver.