

Malawi
In Malawi, we run a comprehensive programme to screen, diagnose, and treat cervical cancer in Bamako, which accounts for 40 per cent of all cancers among women in Malawi. The country has one of the highest death rates for the disease in the world. We also support key medical services for sex workers, such as sexual reproductive healthcare, screening services, and HIV prevention in Dedza and Zalewa.
Our activities in 2024 in Malawi
Data and information from the International Activity Report 2024.
307
307
€5.9 M
5.9M
1987
1987
Featured
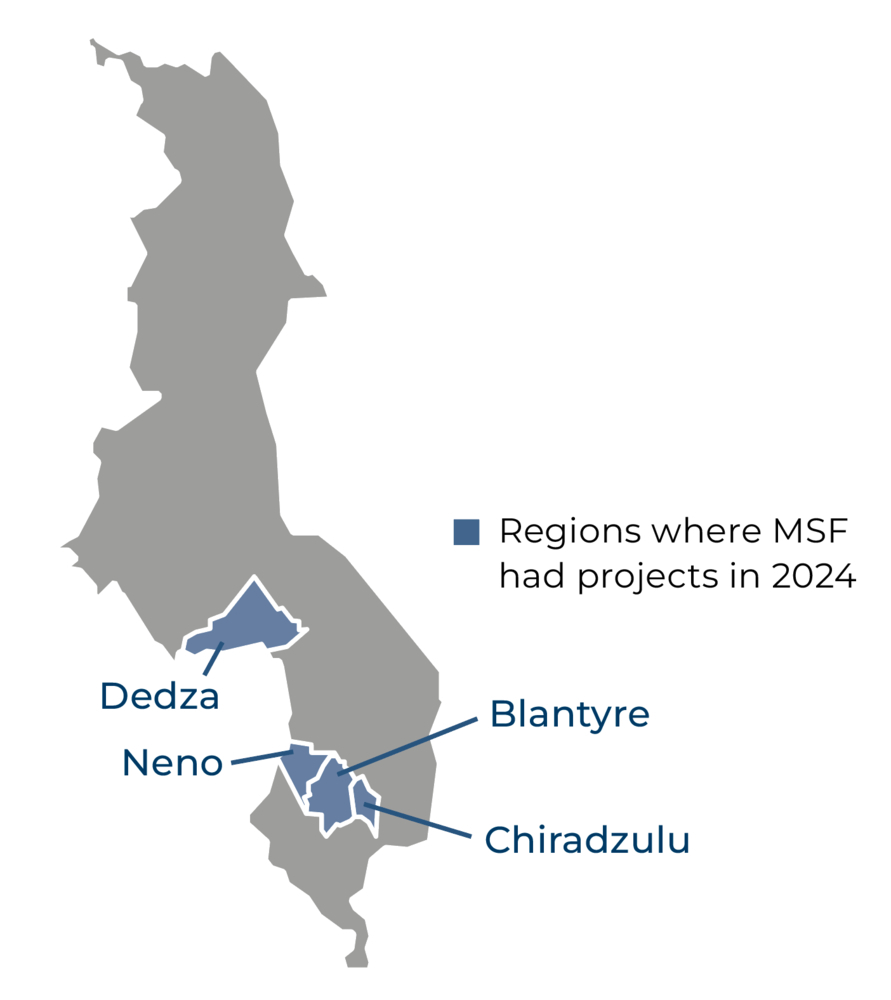
In Malawi’s second-largest city, Blantyre, and the surrounding district, we have worked closely with the health authorities to implement a comprehensive programme that comprises prevention, screening, diagnosis, and treatment, as well as palliative care, for cervical cancer. The disease accounts for almost 40 per cent of all cancers among women in Malawi, and kills over 2,000 each year.
Based in Queen Elizabeth Central Hospital in Blantyre, our services include outpatient treatment for pre-cancerous and cancerous lesions, surgery, chemotherapy, and home-based palliative care for patients in the advanced stages of the disease. Patient-centred activities, such as mental health support, education sessions, physiotherapy, and social support, are also part of our programme.
Prior to 2024, we had to refer patients requiring radiotherapy to facilities in Kenya, as it was not available in Malawi. However, in March, a private radiotherapy centre opened in Blantyre, meaning that patients can now be treated closer to home.
Cervical cancer screening units are integrated into 10 Ministry of Health health centres in Blantyre and Chiradzulu districts, and a mobile screening team also works in Chiradzulu.
In addition to our specialist cervical cancer programme, we work alongside two community-based organisations run by people who engage in sex work in Dedza and Zalewa, providing close-to-home sexual and reproductive health services through mobile outreach clinics. We provide screening and treatment for sexually transmitted infections, cervical cancer screening, contraceptives, information about preventive services for HIV, such as pre- and post-exposure prophylaxis, and mental health counselling.
OUR ACTIVITIES IN 2024

39,100
39,1
19,100
19,1
2,650
2,65
500
5


MSF Prepares to Launch an Innovative Long-Acting HIV Prevention Program in Several African Countries

Treatable Yet So Deadly, Cervical Cancer in Malawi

Sex Workers Take Charge of Their Health in Malawi

MSF closes HIV/AIDS project after 25 years in Malawi

