Young people in South Africa are disproportionately at risk from HIV and are significantly implicated in South Africa’s tuberculosis (TB) epidemic. Additionally, the rate of teenage pregnancy in South Africa is among the world’s highest. Without action to reduce these burdens, they will continue to take a massive toll for generations to come.

Outreach Testing
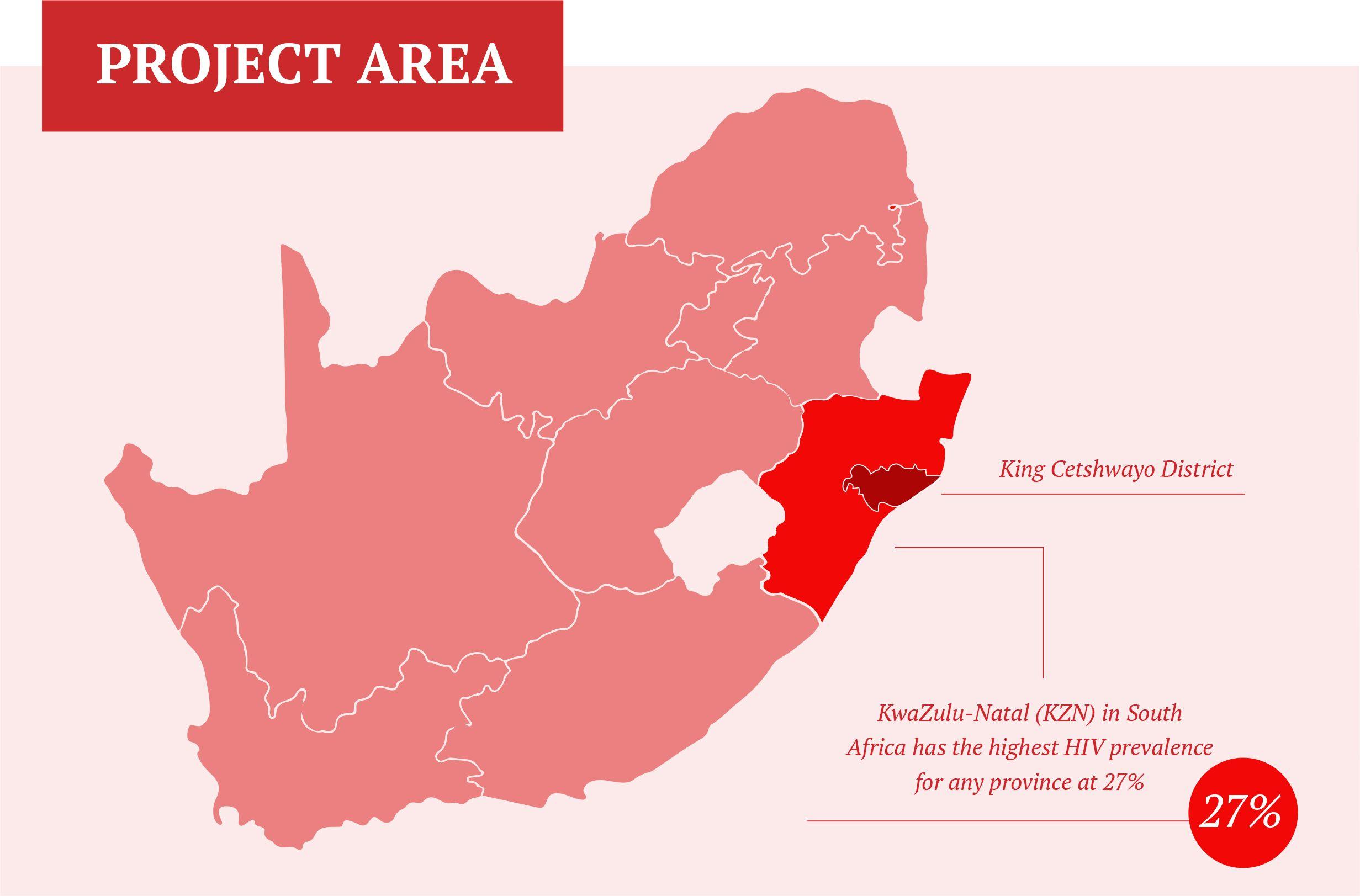
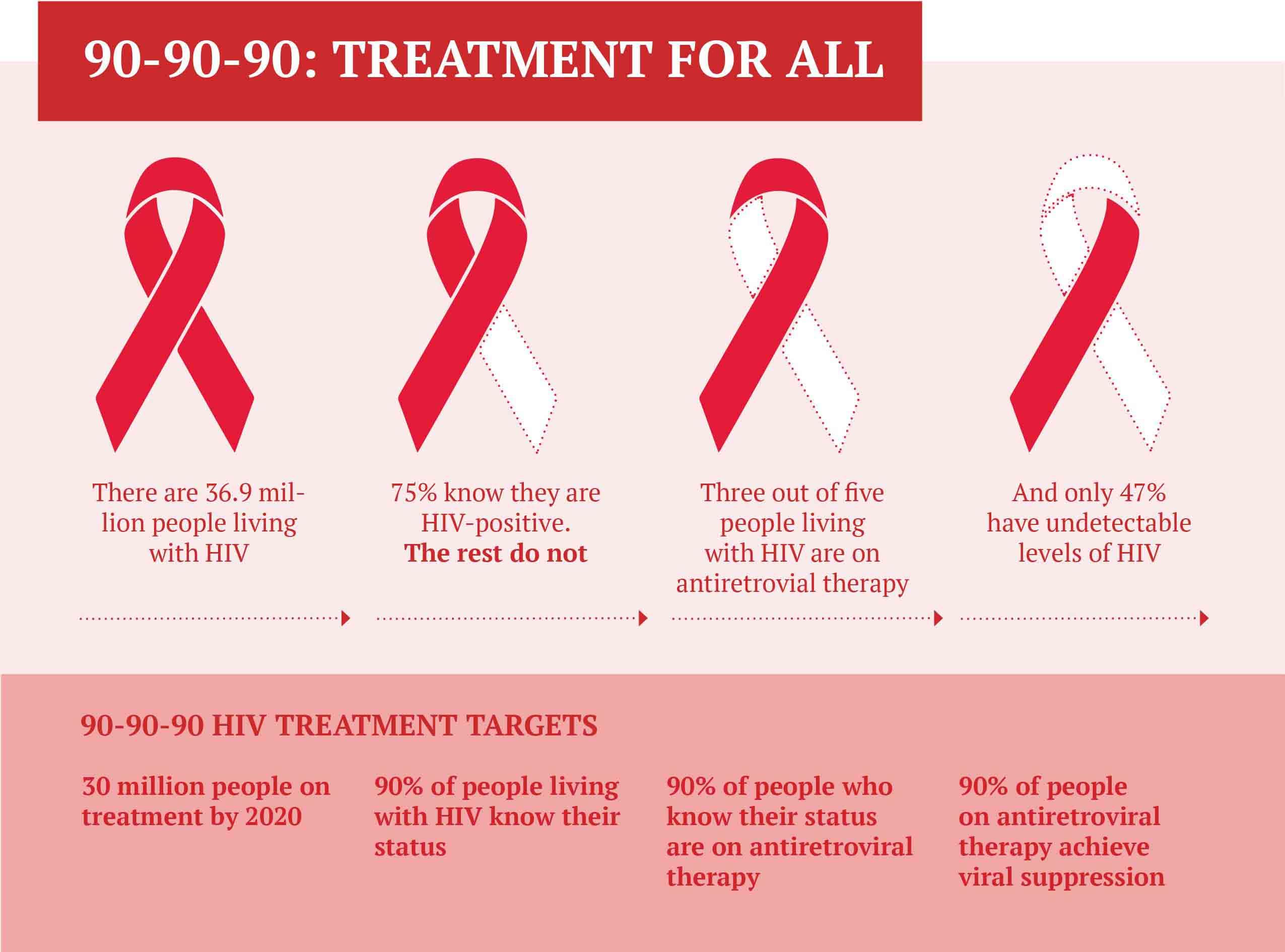
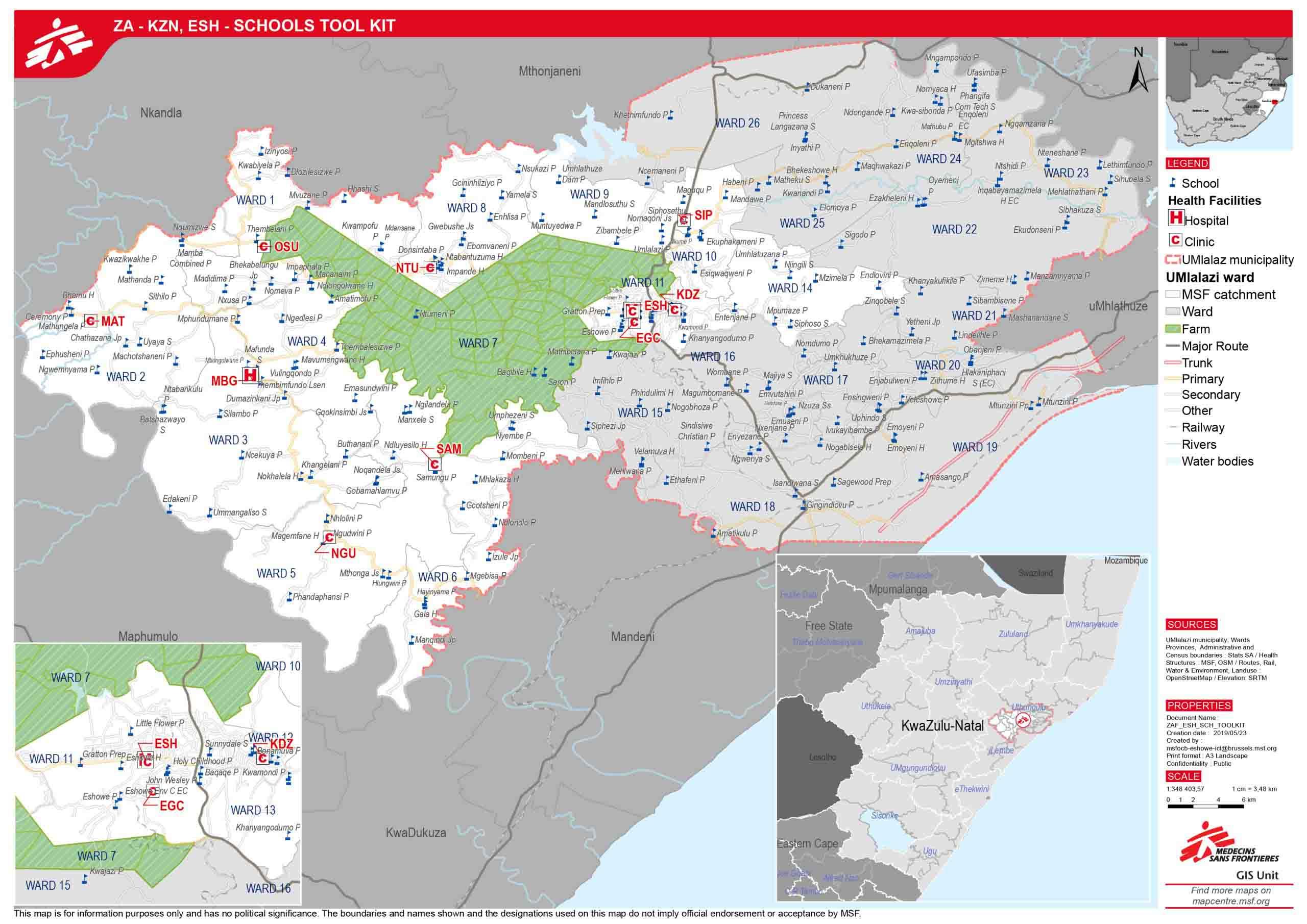
KwaZulu-Natal (KZN) in South Africa has the highest HIV prevalence for any province at 27% [ref: 2018 HSRC HIV Impact Study], and also records the highest number of new TB cases annually. In April 2011, Médecins Sans Frontières/Doctors Without Borders (MSF) in partnership with the KZN Department of Health (DOH) started an HIV/TB project called “Bending the Curves” in King Cetshwayo District (pop. 114 000), aiming to reduce the incidence of HIV and TB, bring down HIV and TB morbidity and mortality, and to help the DoH achieve the UNAIDS 90-90-90 by 2020 targets.
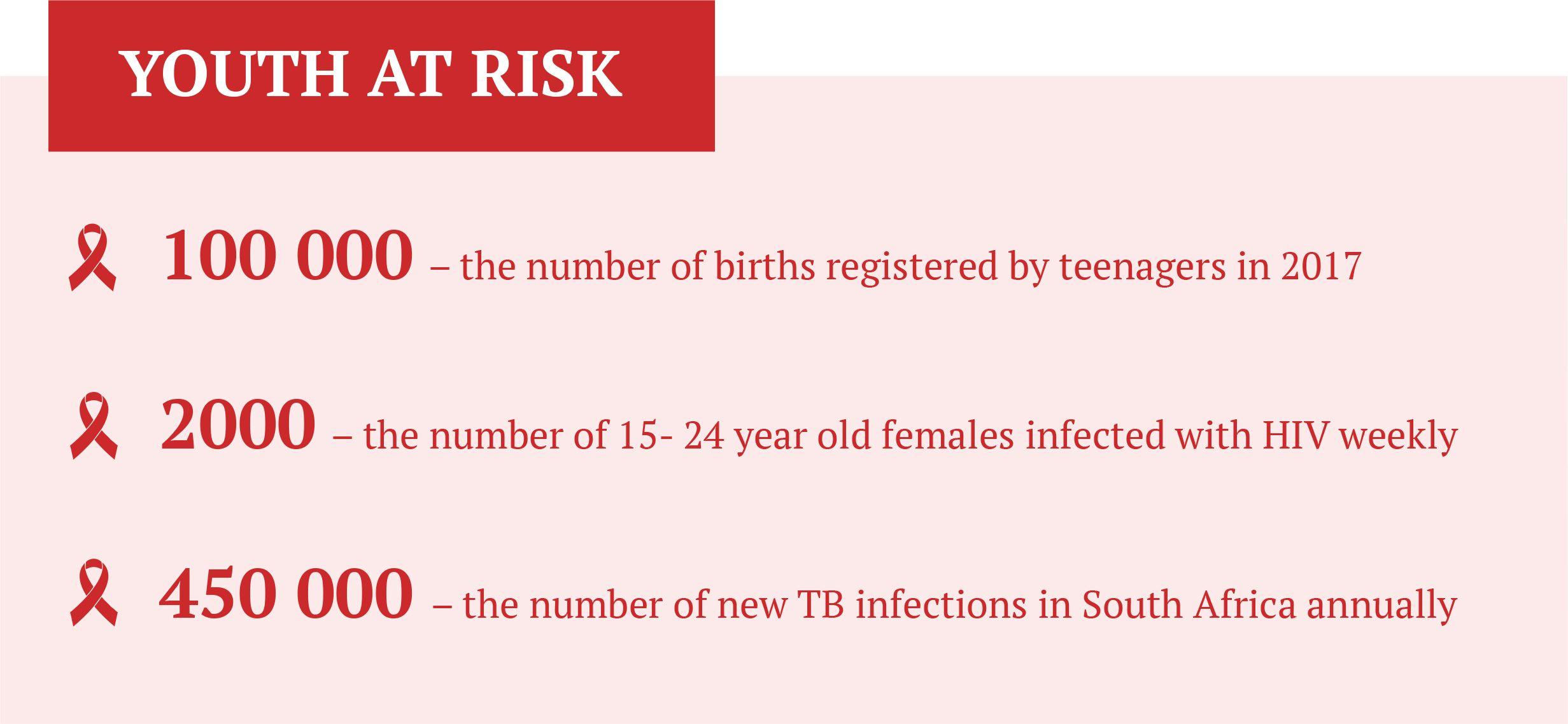
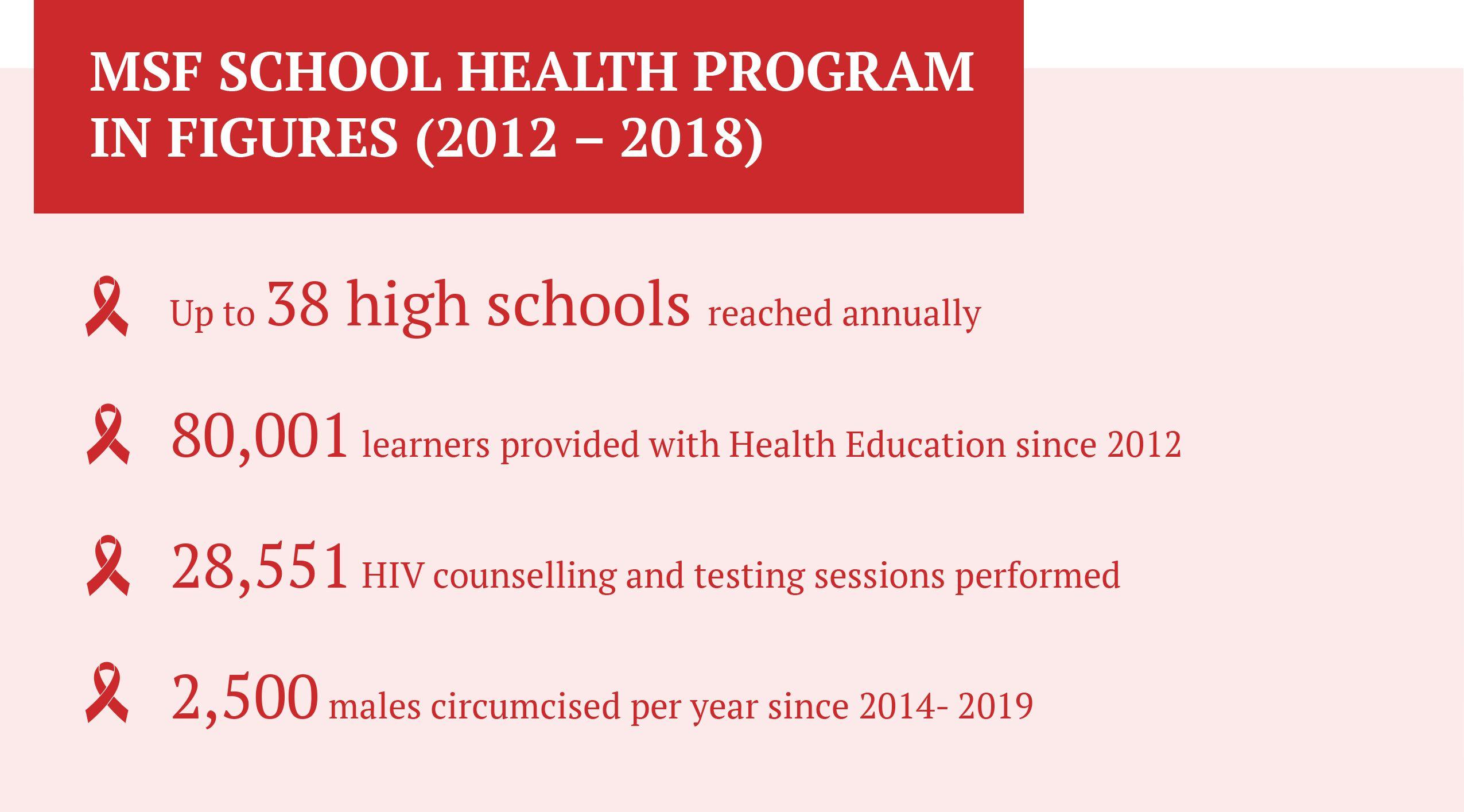
The results of two major studies conducted by MSF made it clear that the HIV epidemic would not be overcome without a strong focus on youth, and with HIV Counselling and Testing (HCT) being the most important entry point for HIV-related prevention, support, care and treatment, MSF embarked on a School Testing Program in 2012 in collaboration with local government, with the aim of reducing new HIV and TB infections while empowering high school learners through education to make informed decisions when it comes to sexual and reproductive health. In time, additional services were offered, and the initiative was renamed the MSF School Health Program.
Analysis of an HIV door to door survey conducted by MSF in 2013 found that 67% of HIV positive men under the age of 25 are unaware of their status, while HIV prevalence in adolescent females was seen climbing from nearly 5% in 18-year-olds to over 20% in 19-year-olds – a clear basis for the provision of Sexual and Reproductive Health (SRH) services in schools [Ref: Mbongolwane & Eshowe Population Survey]
Legal and Policy Framework
South Africa's 1996 Constitution and Bill of Rights protects the right to make decisions regarding reproduction and the right to access healthcare services for both adults and children. Laws such as the National Health Act (2003), the Children's Act (2005) and others give effect to these constitutional rights for adults and children.
The provision of Sexual and Reproductive health (SRH) services to learners is additionally addressed in several national policies and guidelines, most notably the Department of Health’s National HCT guideline, the Standard Operating Procedures for the Provision of Sexual and Reproductive Health, Rights and Social Services in Secondary Schools (hereafter referred to as DBE SOPs) the multi-departmental Integrated School Health Policy (ISHP), and the Department of Basic Education National Policy on HIV, STIs and TB for Learners, Educators, School Support Staff and Officials in all Primary and Secondary Schools in the Basic Education Sector (hereafter referred to as DBE National Policy).

Lack of SRH services in schools leaves teenagers vulnerable to the risk of HIV infections
However, poor alignment of the relevant laws and policies is a significant barrier to service delivery, and there is a need for ongoing advocacy work to clarify grey areas and ensure that adolescents are able to easily access SRH services, especially in secondary schools. Schools are an important entry point because there is a high rate of learner retention in South Africa and, once out of school, it is difficult to reach young people [Ref: The World’s Largest HIV Epidemic in Crisis: HIV in South Africa]. The reality is that school-based SRH services are currently not offered to learners in any of the country’s 9 provinces, with the exception of a handful of school health programs driven by non-governmental organizations.
As the country seeks to implement national policies on school-based health education and services it is important that the evidence and experiences of existing school health programs be accessible to service providers and role-players. It is for this reason that MSF has developed this School Health Program “toolkit”, detailing the approach we followed in developing the MSF School Health Program in King Cetshwayo District in KwaZulu-Natal Province.

The MSF School Health Programme
The MSF School Health Program was launched in 2012 with the KwaZulu-Natal (KZN) Department of Health (DoH) and the Department of Education (DoE), aiming to provide school-based Sexual and Reproductive Health (SRH) education as well as HIV Counselling and Testing (HCT) services for learners and educators in grades 8-12 (age 14 - 18).
The program has annually served learners in up to 38 secondary schools in both urban and rural settings. Uptake of services has been high, with the program’s successes being largely attributable to strong partnerships with the Provincial DoE and the DoH (particularly with the King Cetshwayo District teams), intensive community health promotion efforts, rigorous and ongoing stakeholder consultation, and the fact that services have been school-based and provided in user-friendly ways.
Aims
The Program aims to empower high school learners to make informed decisions when it comes to sexual and reproductive health and to reduce new HIV & TB infections by:
- Providing information on HIV/TB and HIV/TB prevention, and informing learners about proactive steps they can take towards a healthy lifestyle, irrespective of HIV status;
- Mobilizing learners to use the program’s HIV Counselling and Testing (HCT) services.

Services
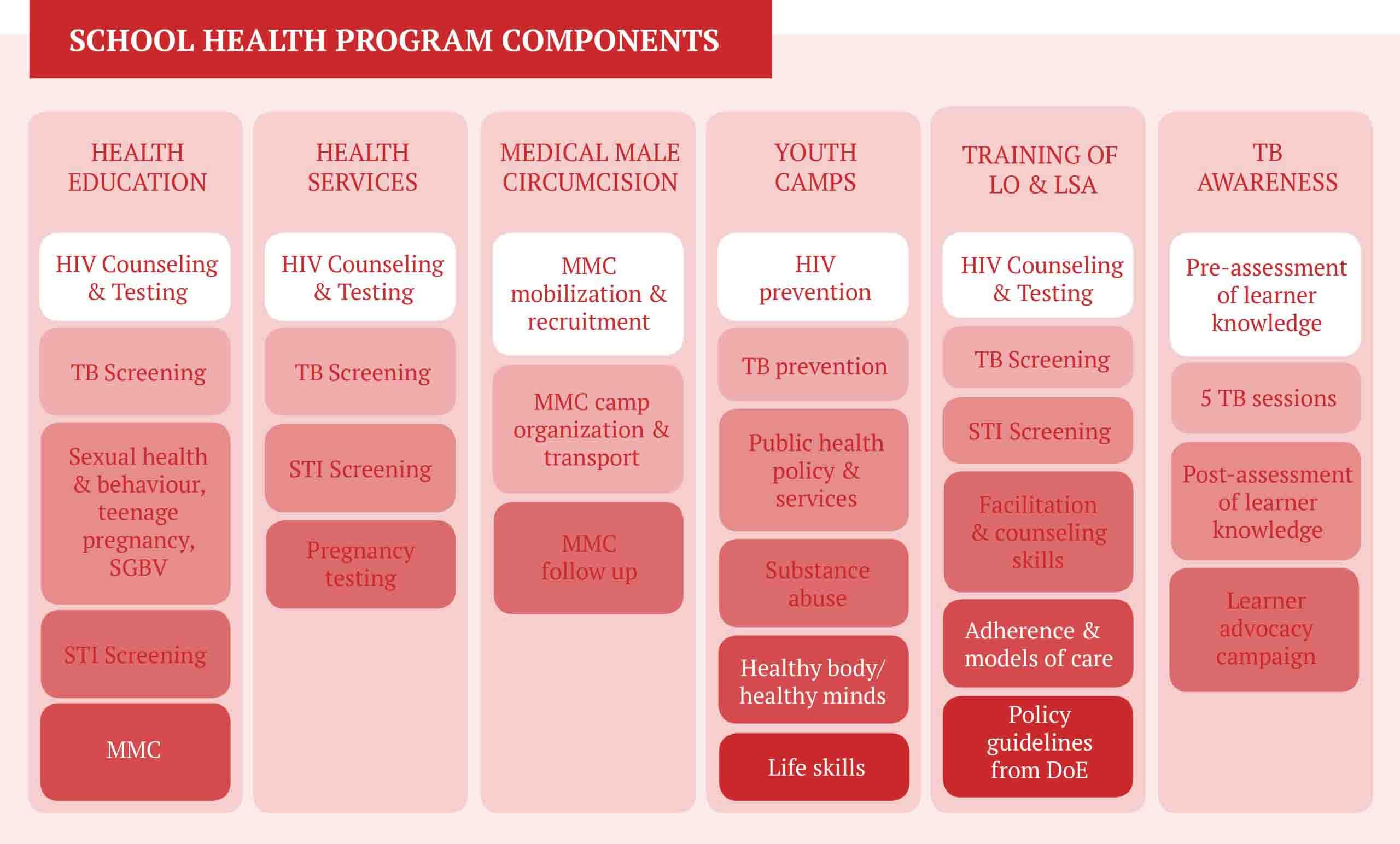
HIV is the biggest health issue for youth in South Africa. HCT is the most important entry point for HIV-related prevention, support, care and treatment, and therefore these services lie at the heart of the MSF School Program offering. The full package of services includes:
- Age-appropriate health education, pre-approved by the DoE, to inform high school-age children about their sexual reproductive health, HIV, TB, and the importance of knowing their HIV status
- Provision of SRH Services, including HCT, provision of condoms and screening for STIs, TB, and pregnancy;
- TB Awareness Campaign, comprising comprehensive TB education and a learner advocacy campaign.
- Training of Learner Support Agents (LSAs) and Life Orientation Educators (LOs), towards reducing in schools and ensuring that learners have access to year-round support in regard to sexual and reproductive health matters.
- Information on Medical Male Circumcision (MMC) and recruitment for MMC camps run in collaboration with the DoH.
- Youth health camps for select learners, comprising dialogues on SRH matters that help to keep the School Health Program attuned to what learners want from services, and as a means of empowering select learners to carry information on sexual and reproductive health to their peers.
Section 2.6 of the Integrated School Health Programme outlines a comprehensive package of health and social services that should ideally be provided to learners on school grounds, ranging from parasite control to immunizations to SRH services such as HCT and screening for STIs. The MSF School Health Program was designed to meet a particularly urgent need for HIV services and does not provide the comprehensive package of services as defined in the ISHP. It is envisaged that the full package of services will be provided by many actors, and MSF recommends that where it is not possible to offer comprehensive health services to learners HIV services should be provided at the minimum, given the scale of the HIV crisis in South Africa.

Partnerships
Strong partnerships with a range of governmental and civic society actors are the bedrock of any successful school health program, especially in South Africa where conservative parent/educator opposition remains the single greatest barrier to the roll-out of school-based SRH services. The following partnerships have been integral to the success of the MSF School Health Program:
Department of Education, specifically
- DoE officials in charge of Life skills and implementation of the school health program (local, provincial and national) such as Provincial Chief Educational Specialist, District Special Needs Program Coordinator.
- School Governing Body (SGB): a statutory body of parents, educators, non-teaching staff, principal and learners (from Grade 8 or higher) who seek to work together to promote the well-being and effectiveness of the school community and thereby enhance learning and teaching.
- Learner Support Agents (LSA): Department of Education employees providing social and psychosocial support to all learners in high schools and primary schools.
- Life Orientation Teachers (LOs): Qualified teachers employed by the DBE to lead learners in the study of the self, and what it means to be a responsible, healthy member of a democratic society.

Department of Health
- DoH School Health Program: MSF collaborates with the DoH Schools Health Unit on certain calendar events, providing health services such as HCT at these events and occasionally supporting health education sessions.
The Department of Social Development
- Social Workers: Provinces are divided into Districts, which are in turn divided into wards. The DSD employs social workers in all wards, and the MSF School Health Program refers psycho-social cases to the ward social workers.
Non-governmental organizations
- Impilonhle: an Organization providing training for LSAs and LOs, as well as study group and homework support to learners.
- One Voice South Africa: an Organization providing training on TB, including the training of LSAs, LOs and peer-educators.
- Shintsha Health Initiative (SHINE): a Community-based Organization providing health education for learners and mobilization for MMC.

Co-ordination of role-players
Representatives of all partners involved with the MSF School Health Program sit on a School Health Steering Committee, which meets quarterly, chaired by the DoE District Coordinator of the life skills program, with the Coordinator of the DoH Hospital-based School Health Program as Deputy Chair.
Committee members share achievements, discuss challenges and draw up operational plans for the coming quarter. These meetings also serve as a platform for the sharing of strategies by new partners and potential partners.

Staff
Each school visit requires the deployment of 2 lay counsellors, 2 Health Promoters and 1 driver. Depending on the size of the school and the number of learners wanting to be tested additional counsellors might be required.
Lay Counselors: Members of the community trained to perform patient support and education tasks for HIV and TB. Lay counsellors with the MSF School Health Program provide SRH education to learners, as well as HCT services.
Health Promoters: Members of the community trained to recruit learners for HCT and MMC, helping to develop and implement health education and health promotion programs. On the day of testing at schools, health promoters motivate learners in the testing queue, ensure that learners do not wander off, and fiercely emphasize the importance of keeping results confidential. Health promoters are a year-round source of health information and support for learners, and they provide sustained support to male learners who have undergone MMC.
Drivers: transport program staff and materials to schools and help to set up activity installations.

Implementation
Engaging with communities and education role-players
Implementation
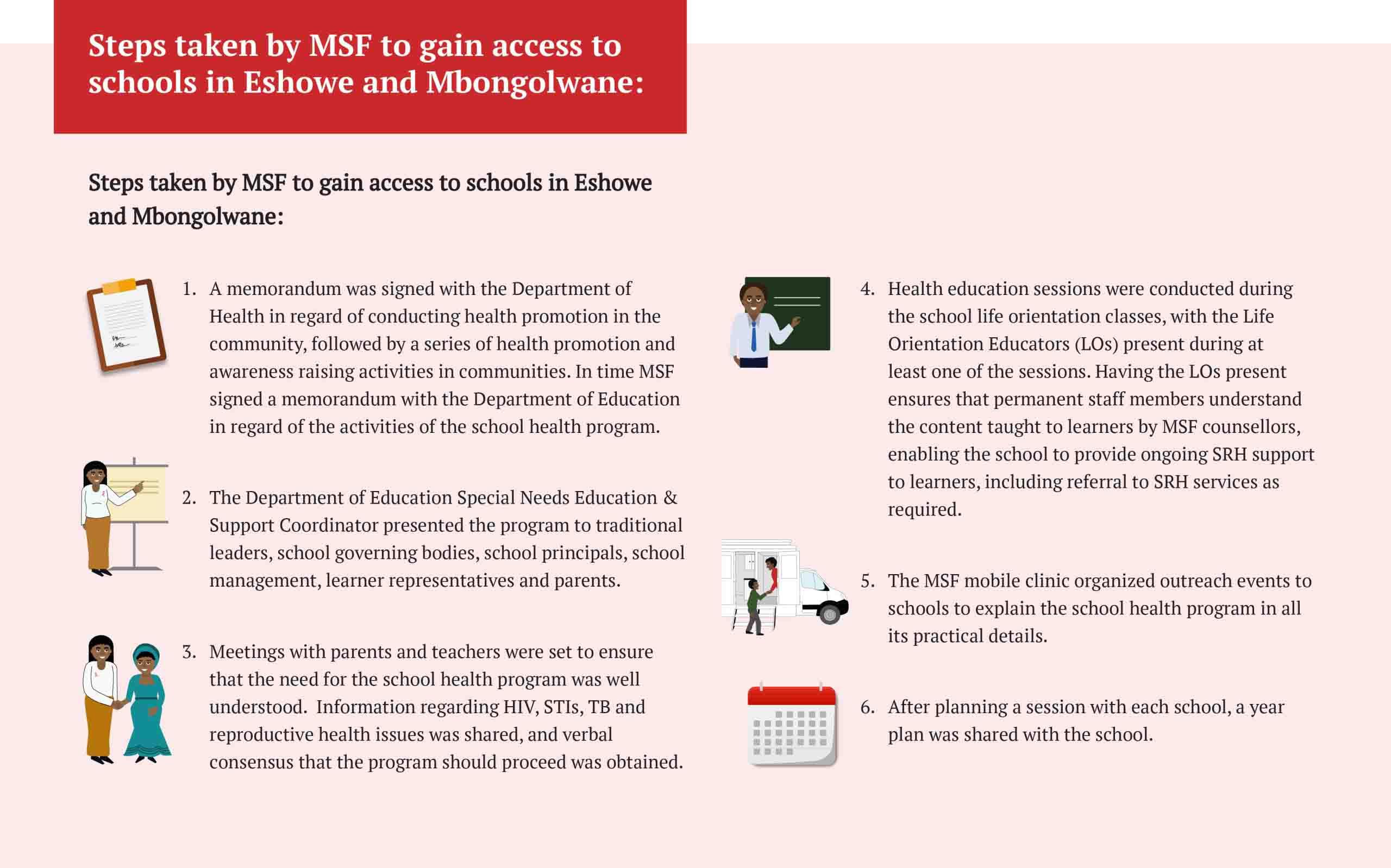
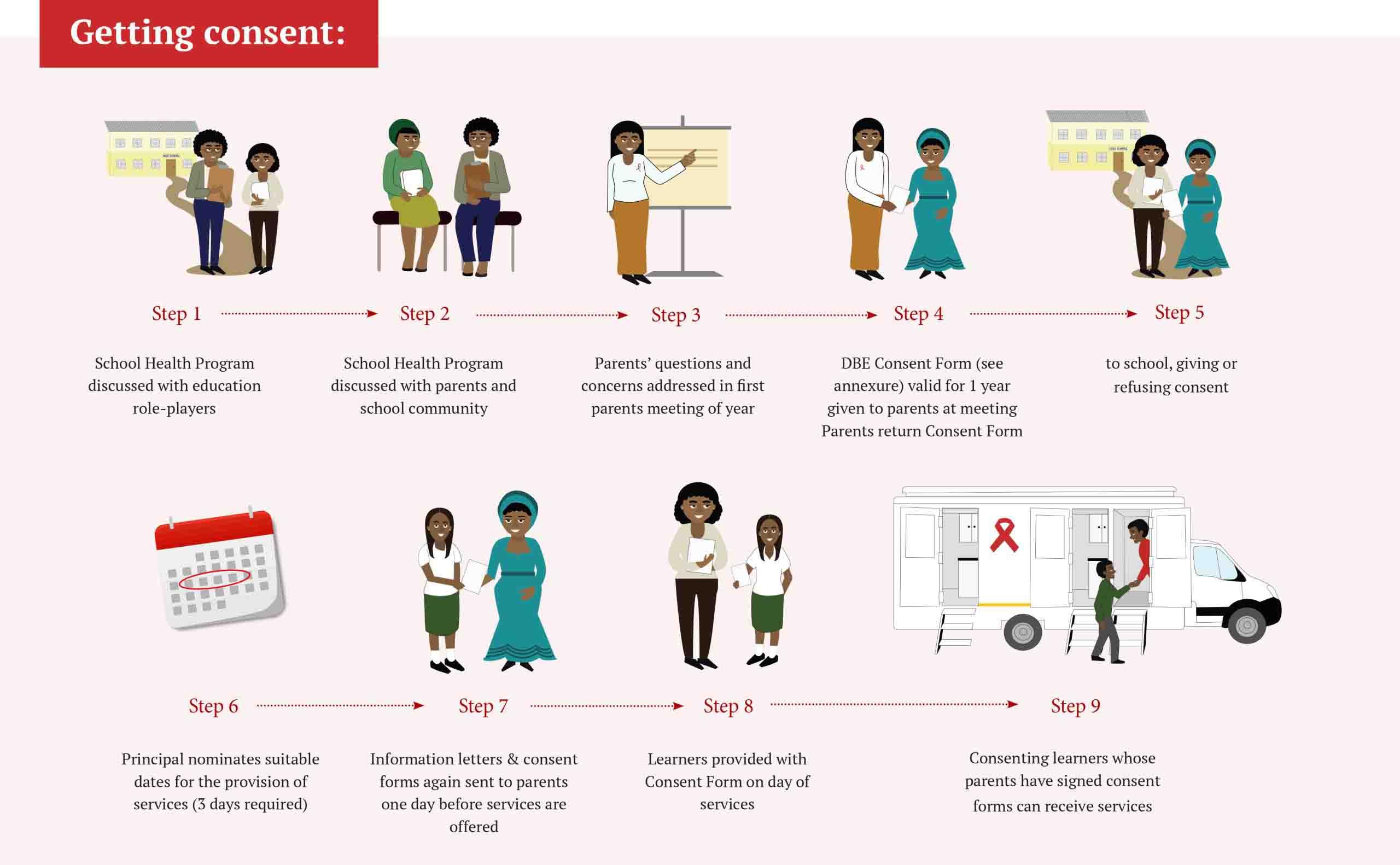
Meaningful community engagement is vital when it comes to the provision of Sexual and Reproductive Health (SRH) services in schools. The DBE National Policy stipulates that learners wishing to use school-based SRH services must first obtain the informed consent of a parent/guardian. Part 4.3 of the DBE policy implementation guideline (DBE SOPs) recommends that a rigorous process of educator/stakeholder engagement should precede any appeal for parental/guardians to consent for a learner to access SRH services.
This is consistent with MSF experience. Before launching the School Health Program in King Cetshwayo District, MSF took care to secure the support of the DBE district management and several school principals before proceeding to organize parent meetings at which the program was explained in detail. Many parents contested the program initially, and this prompted MSF to organize a series of health promotion activities in communities, highlighting the impact of HIV on the youth in the district and explaining the potential health benefits of school-based testing. Community health workers went door to door and stressed the importance of testing, especially for young people.
Sensitising school communities
'We realized the time was right to offer school-based testing when parents started asking our fieldworkers to come back and test on Friday afternoons, when their children would be at home,' recalls Ntombi Gcwensa, a Patient Support Activity Manager with MSF. With meaningful community engagement the MSF School Health Program was able to enter schools and successfully offer HIV Counselling and Testing (HCT)and other SRH services to learners.

Community Health Agents Programme - CHAPS
Planning a School Visit
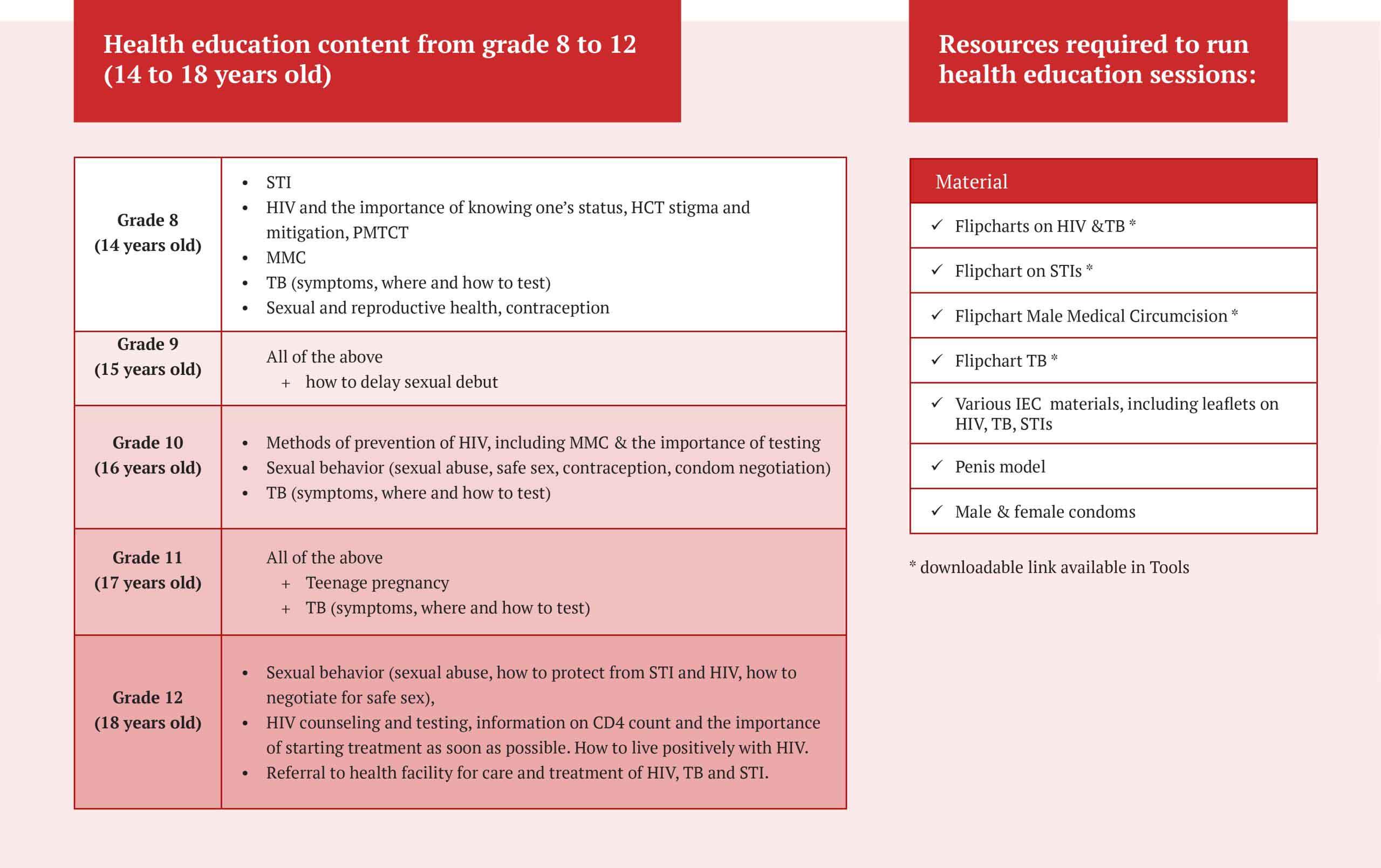
The number of days spent in each school varies according to the size of the school and the number of learners recruited for HCT. Typically, the team spends 2 – 3 days in a school, with up to two days for education sessions in classes, and a day for the delivery of HCT and other health services inside the mobile health unit. At least one day before each planned visit the MSF School Health Program Manager will call either the school principal or the life orientation educator (LO) to confirm the arrangement. The lesson plans are discussed with the LO, who is asked to schedule a 45 -60 minute health education lesson for all classes in Grades 8 - 12.
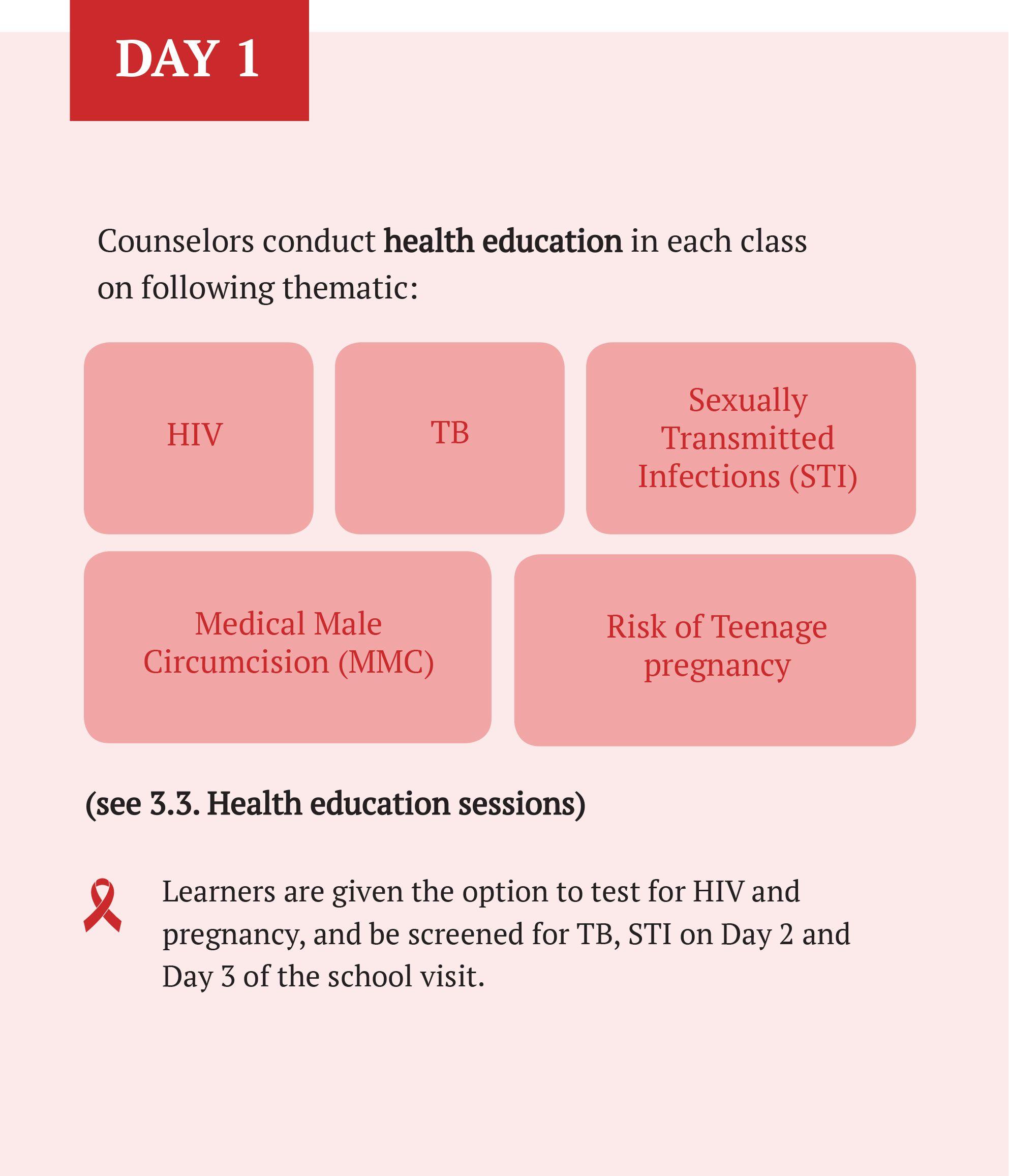
Counsellors conduct health education in each class on following thematics:
- HIV
- TB
- Sexually Transmitted Infections
- Medical Male Circumcision (MMC)
- Risk of Teenage Pregnancy
Learners are given the option to test for HIV and pregnancy, and be screened for TB, STI on Day 2 and Day 3 of the school visit.
Counsellors conduct a one-on-one session providing:
- HIV testing
- TB screening
- STI screening
- MMC Recruitment
- Pregnancy test
Learners willing to benefit from services should be able to provide written consent from their parents or guardians. However, the school principal can also provide written consent if the learner is willing to test.
Screening for TB and STI is followed by referral to the nearest clinic for further examination as required.
Consent
Knowing what consent is required before SRH services can be offered to learners is very important. The Children’s Act (2005) gives children aged 12 and older the right to take an HIV test and to access contraception without adult consent. However, MSF experience strongly indicates that successful implementation of SRH services in schools is not possible unless parents are thoroughly consulted and their 'buy-in' is broadly secured.
Nationally, there have been cases where the alleged failure of providers to secure parental consent to test learners led to the suspension of school-based testing services. In addition to the MSF process depicted below, Providers are advised to closely follow the guidance on Consent set out in section 4.3 of the DBE SOPs.
Contradictory Laws and Policies
In addition to following DBE guidance providers should receive training on the laws and policies guiding the provision of SRH services to learners, as poor alignment has given rise to significant operational grey areas, some of which expose Providers to potential legal implications.
For example:
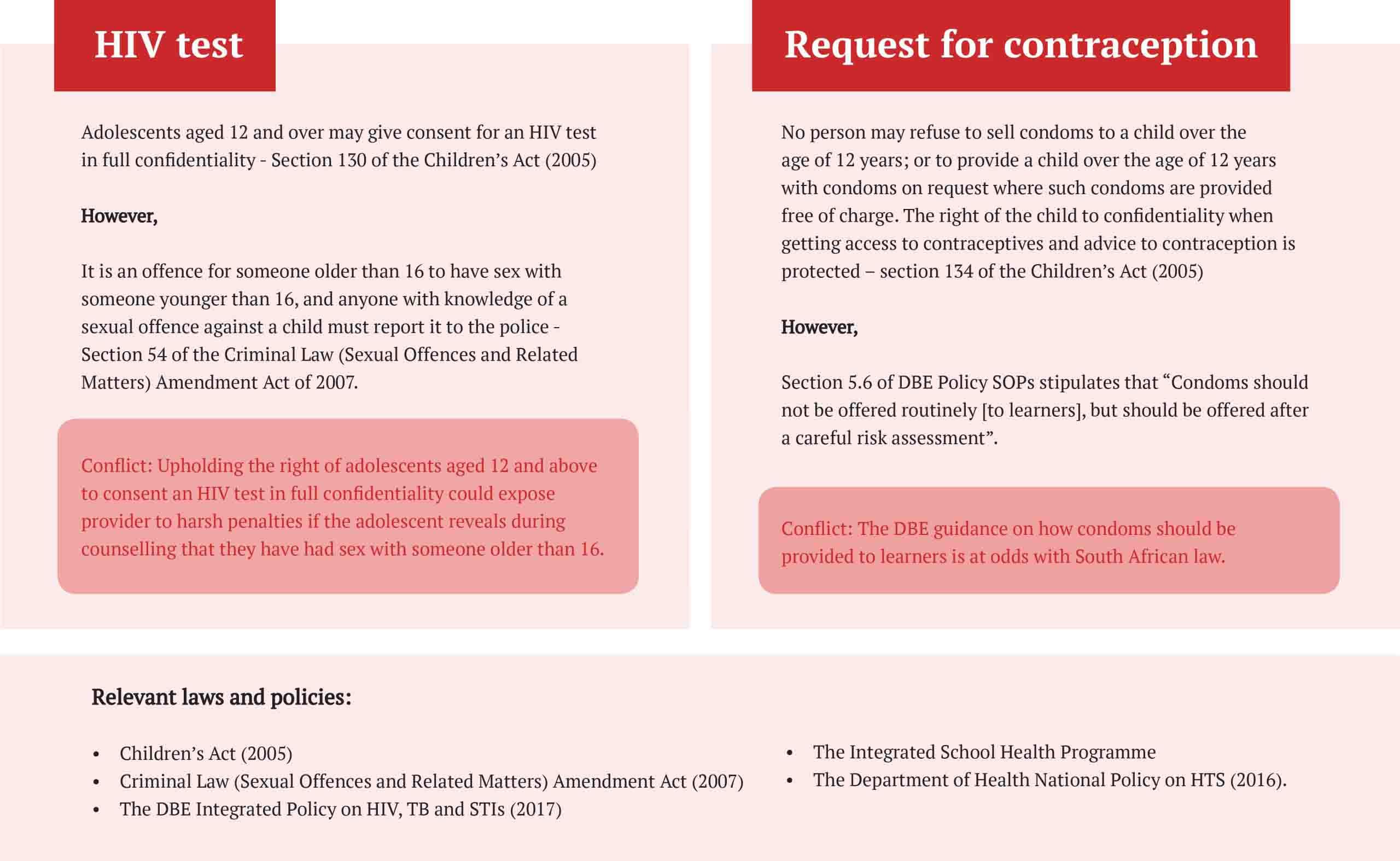

Lack of SRH services in schools leaves teenagers vulnerable to the risk of HIV infections
Implementation of Services
Health education sessions
On the morning of Day 1 when the team arrives at the school, the senior MSF counsellor pays a visit to the school principal to confirm that activities can proceed. The principal typically calls the Life Orientation Educator in at this point, requesting that this staff member provide the school health team with a schedule of the day’s health education sessions and ensure that the schedule is shared with teachers.
MSF counsellors are allocated specific classes in which to provide SRH education. Sessions are 45-60 minutes and can be longer, depending on how interactive the learners are. Health education sessions are drawn from the DBE life orientation curriculum, and cover topics such as HIV and TB prevention, HIV/TB treatment, teenage pregnancy, Sexual and Gender-Based Violence, and more.

In the experience of MSF, the level of learner engagement will depend to a significant extent on the quality of the educator. MSF employs lay counsellors to provide education sessions, and according to Patient Support Supervisor Nosicelo Ntumase, ‘What we look for in a counsellor is someone who is out there - very friendly and fun, but who can also command respect.’ MSF counsellors undergo training on how to conduct health education games, and how to engage learner interest.
Experienced MSF counsellor Jabu Mthimkulu advises that ‘Teenagers aren’t little adults, and if you want to engage learners on sexual and reproductive health matters you need to think as they do.’ Mthimkulu incorporates social theatre in her lessons, believing that, ‘learners listen when you hold a mirror up to their lives.’ If the school is large it can take two days to complete education sessions. Flexibility is essential, as bad weather and changes in school routine around examination times can require postponement.

TB education sessions
The health education sessions delivered by MSF School Health Program exposed a low level of knowledge around TB. The current Life Orientation Curriculum does not deliver adequate information on TB, and for this reason, MSF launched a TB education initiative in 2018, working in partnership with the District DBE and One Voice South Africa, an NGO in Durban that has implemented a similar TB intervention in Durban High Schools. A major preparatory element of the initiative was comprehensive TB training for selected educators. 16 LOs and 16 LSAs from 13 high priority areas attended the training.
MSF identified 13 high schools in 6 wards - identified as 'high priority' by the DoH - in which to roll out school-based TB education. One Voice South Africa provided training to MSF counsellors on how to conduct the TB education sessions, working from a TB Workbook developed by MSF in partnership with One Voice South Africa and the DBE. The TB Workbook (See Tools) covers 5 TB sessions to be presented in the classrooms of the identified 13 schools. Orientation sessions were held with the relevant school principals and post-session questionnaires are conducted as a means of evaluating impact. In 2020 the TB education initiative will be expanded to the remaining schools covered by the MSF School Health Program
Health Services
TB, STI, Pregnancy screenings
Before starting the screening session the counsellor will ask if the learner understood the previous day's education session covering information on TB, STIs, HIV and more. If the learner has questions or knowledge gaps, the counsellor will assist.
TB screening:
The counsellor asks each learner the following questions, and if the answer is 'yes' to one or more the learner is referred to a specific health worker based in the nearest health facility.
- Have you suffered any unexplained weight loss recently? (Have you noticed that your clothes are looser than usual, even though you haven’t changed your dietary habits?)
- Do you have a cough that you are worried about?
- Do you have night sweats, even when it’s cold?
- Do you have feverish symptoms?
- Do you suffer from loss of appetite? (Are you often not hungry, even if you have had nothing to eat all day?)
STI screening:
During the STI screening, the counsellor asks the following questions, and if the answer is ‘yes’ to one or more of the questions the learner is referred to a specific health worker, based in the nearest health facility.
- Have you experienced any pain in your genital area?
- Do you experience any pain when you urinate?
- Do you experience any itchiness in your genital area?
- Do you suffer from any genital sores or warts, whether painful or not?
- Have you noticed any discharge from your genitals (smelly with a dark, brownish colour)?

Pregnancy test:
For pregnancy screening the counsellor asks the following questions, and if the answer is ‘yes’ to one or more of the questions the client is offered a pregnancy test.
- When was the last time you had unprotected sexual intercourse?
- When was your last menstruation?
- When do you usually get your periods?
- Are you experiencing any changes in your body?
Learners answering ‘yes’ are given a test kit and shown how to use it, so that they may test in privacy. It is important to clarify to the learner that the accuracy of the result depends on the time that has lapsed since they last engaged in unprotected sex. Once the learner has tested, she returns to the counsellor and the learner and counsellor read the result together.
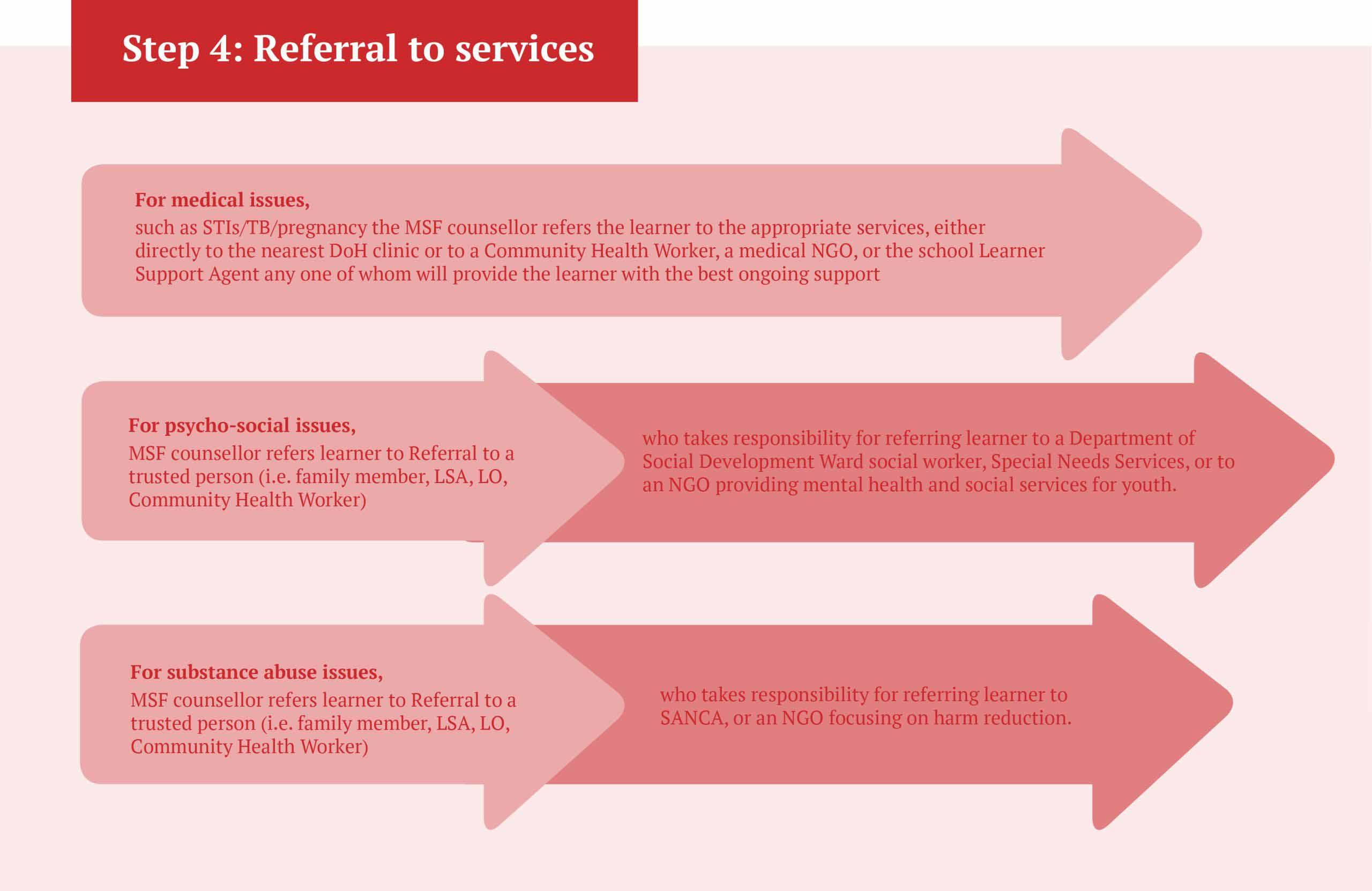
Referral:
For medical issues such as STIs/TB/pregnancy, the MSF counsellor refers the learner to the appropriate services, either directly to the nearest DoH clinic or to a Community Health Worker, a medical NGO, or the school Learner Support Agent - whoever will provide the learner with the best ongoing support.

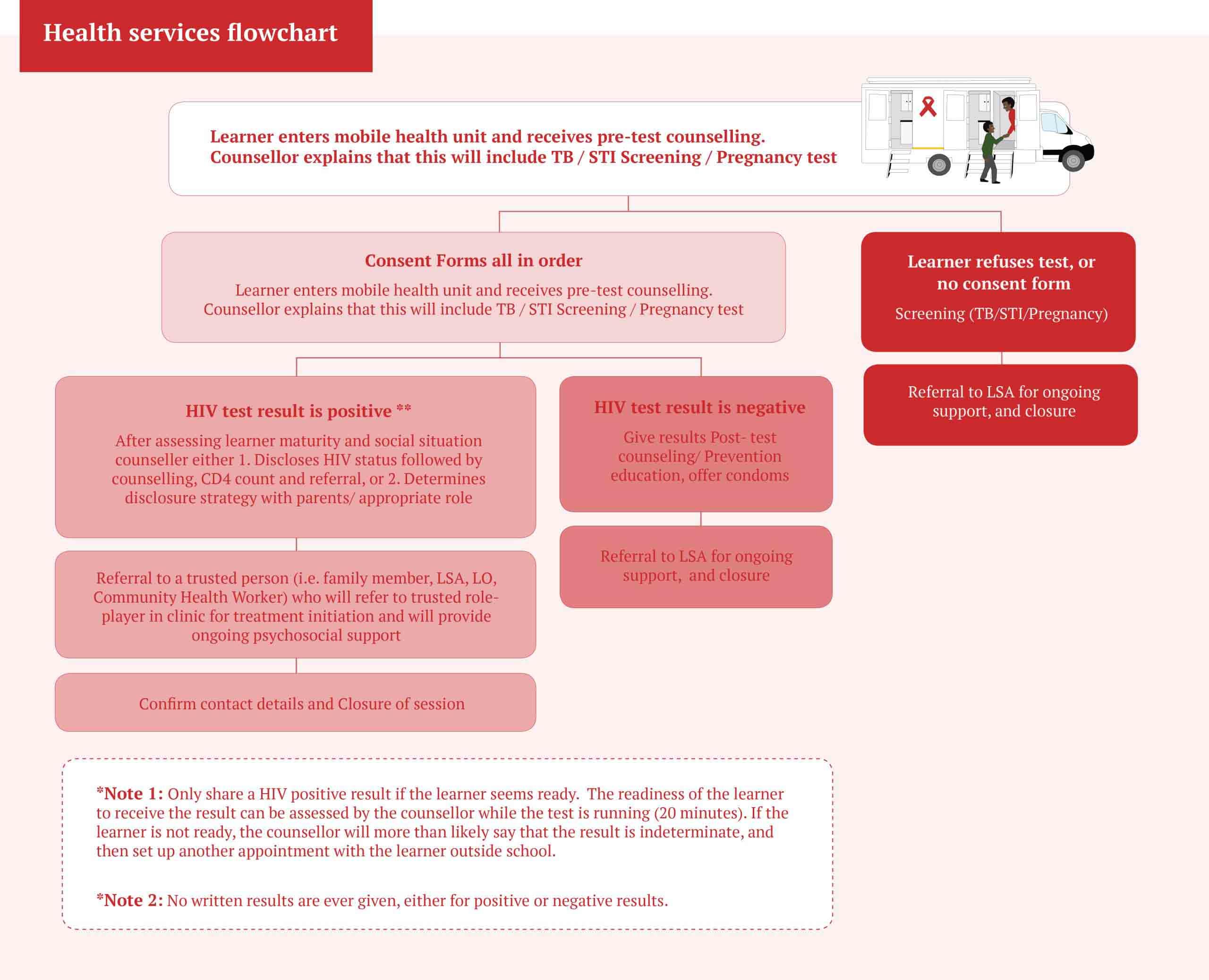
Sexual reproductive health: HIV testing and counselling in schools
HCT is the main service offered by the School Health Program. It is available to consent learners aged 12 and above who can additionally provide written consent from a parent or caregiver (see note on consent).
HCT encompasses:
- HIV counselling session with a qualified counsellor
- HIV test
- Point of care CD4 Count for those who test HIV Positive
- Formulation of an approach to disclosure
- Referral to a health facility for care and treatment
HCT process:
Step 1: Learner receives pre-test counselling, following process outlined in Section 6.2 of the DBE SOPs.
Step 2: Learner is tested, following process outlined in Section 6 of the DoH SOPs, as well as Sections 5/6 of the National HIV Counselling and Testing Policy Guidelines.
Step 3: Communication of test result and post-test counselling. Refer to section 4.3/4.4 of the DBE SOPs as well as the DoH Disclosure Guidelines for Children and Adolescents in the context of HIV, TB and non-communicable diseases
Disclosing HIV status to adolescent learners is one of the greatest challenges faced by providers of school-based SRH services. It entails telling individuals who are undergoing major physical and emotional changes that they have a sexually transmitted illness that is potentially life-threatening and highly stigmatized.
Unsurprisingly, parents and healthcare providers often have differing views about when and how to share such difficult news [ref: Ethical Issues Concerning Disclosures of HIV to Perinatally Infected Children and Adolescents]. This is often the case when the learner has been perinatally infected. When there is a strong chance that a learner has been perinatally infected – for example, if the learner informs the provider that they have taken medicine daily for as long as they can recall but do not know what the medicine is for – the provider is faced with some difficult ethical questions. According to the Children’s Act (2005), any adolescent aged 12 or older has the right to test and confidentially learn their HIV status.
However, disclosing to a perinatally infected child could compromise the mother’s own right to confidentiality. In King Cetshwayo District and elsewhere there have been cases where alleged disclosure to perinatally infected learners has led to an outcry and the suspension of school-based HCT services. The legal and policy framework around disclosure to children and adolescents provides some guidance to providers but it is not definitive, leaving providers with the difficult job of determining an approach to disclosure that navigates conflicting laws and policies while remaining sensitive to the specifics of the case. This is a high burden of responsibility and providers must be adequately trained to manage the disclosure process.

Good referral pathways are an essential part of any successful school health program. When referral pathways are weak it can delay access to appropriate care and lead to health consequences and negative impacts that could have been prevented or lessened with a timely referral.
The MSF School Health Program benefits from the fact that the MSF works at every level of healthcare in the King Cetshwayo District, meaning that our counsellors are able to directly or indirectly refer learners to individuals in the health system they know and trust. Referring a learner to a nearby facility or organization is simply not enough, as there is a high chance that the individual will feel intimidated and may not present for care.
Not all providers of school-based health services will have access to such ready-made referral networks. A good strategy for developing a strong referral network is to establish a stakeholder working group, comprised of organizations in the project area that also work in healthcare. This way providers can map the available services in the area, and use the working group platform to develop specific referral pathways.

For optimal results, MSF experience indicates that school-based health services should be based on school grounds and offered during school hours. DBE policy allows for this if services are offered in a way that ensures privacy, and do not disrupt school activities.
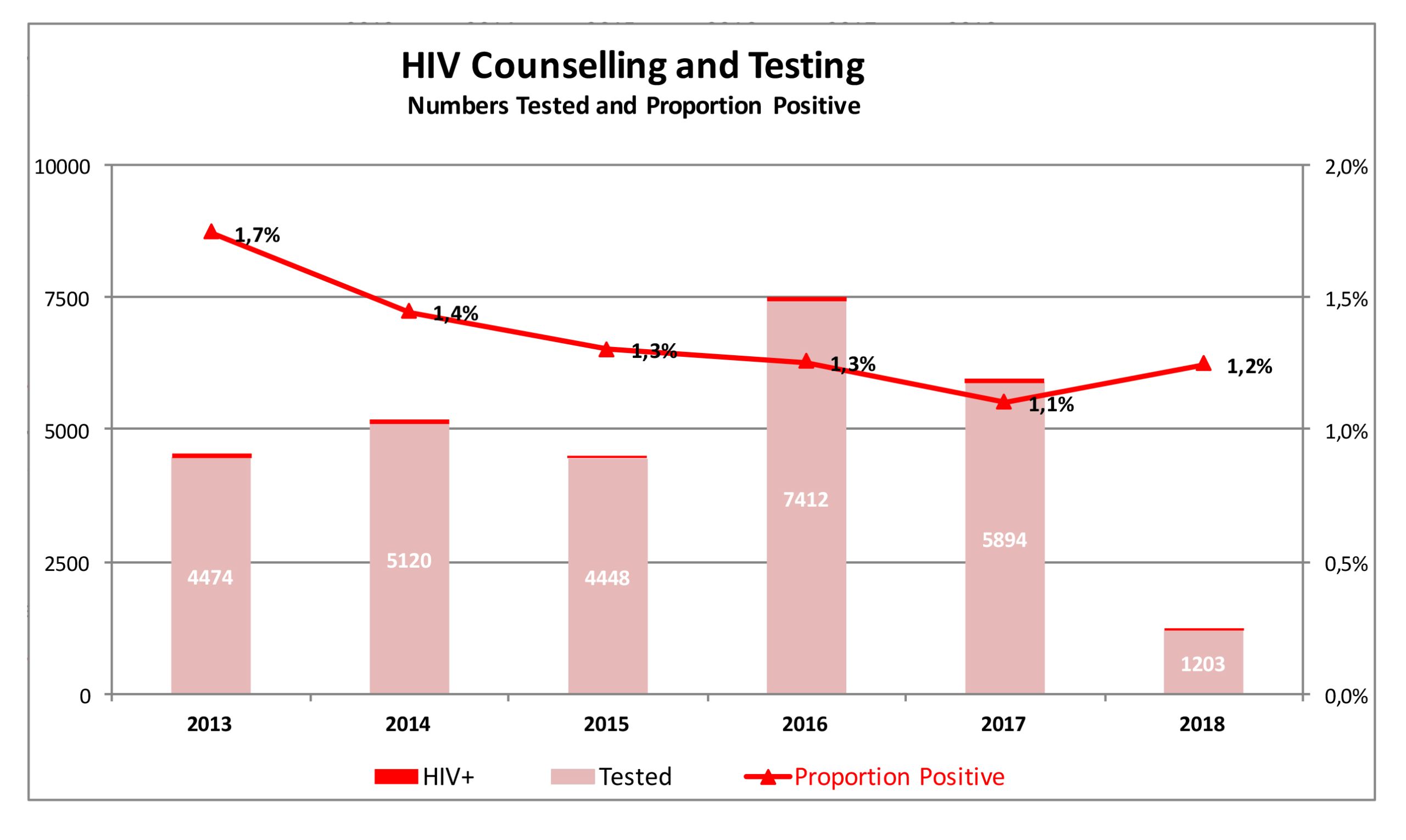
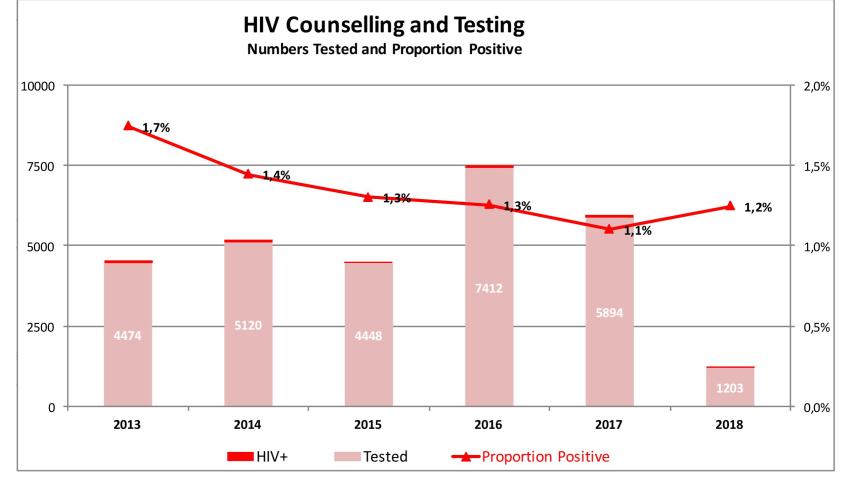
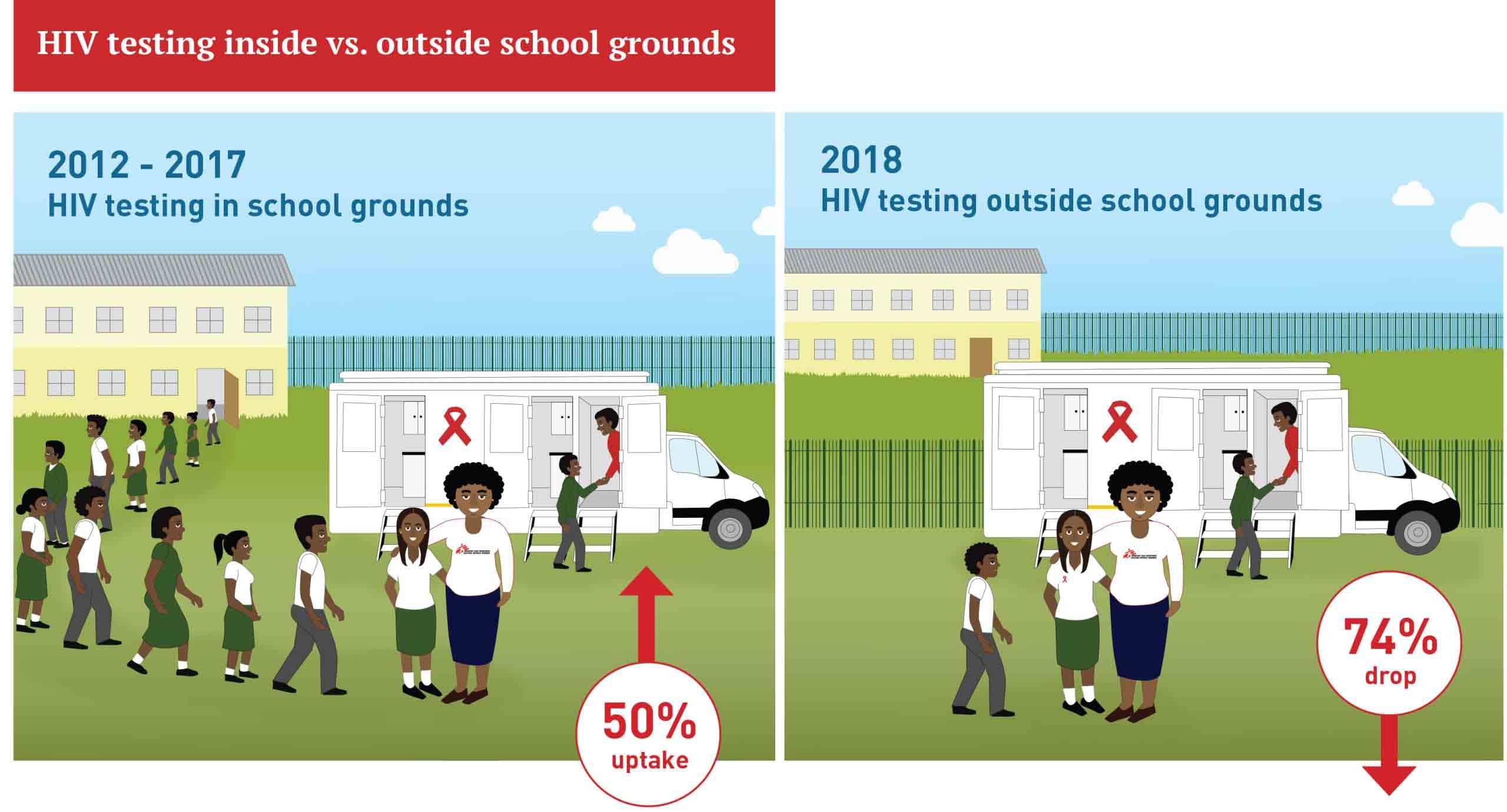
From 2012 to the end of 2017 MSF successfully offered HIV testing in up to 38 schools in King Cetshwayo District, operating within school grounds and during school hours. In 2017, MSF was able to test 5,894 learners this way. However, in 2018 when the district DoE asked MSF to offer health services outside the school gates only 1,203 learners were tested, representing a 74% drop in coverage!
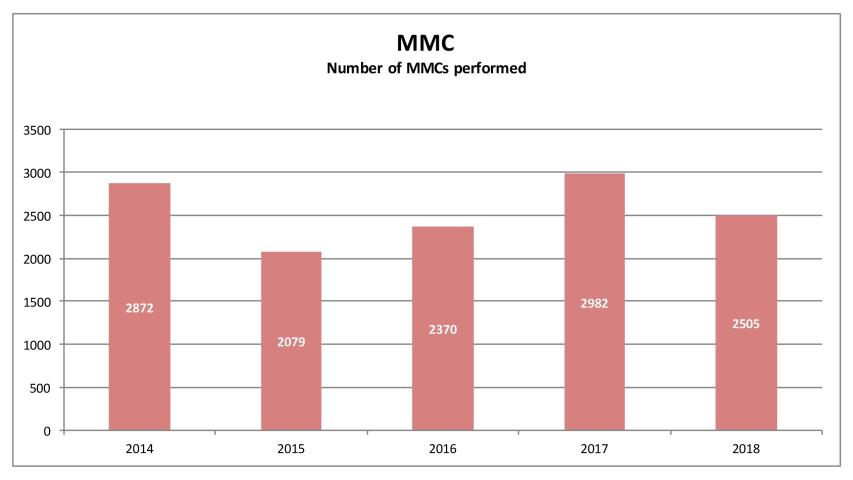
Medical Male Circumcision
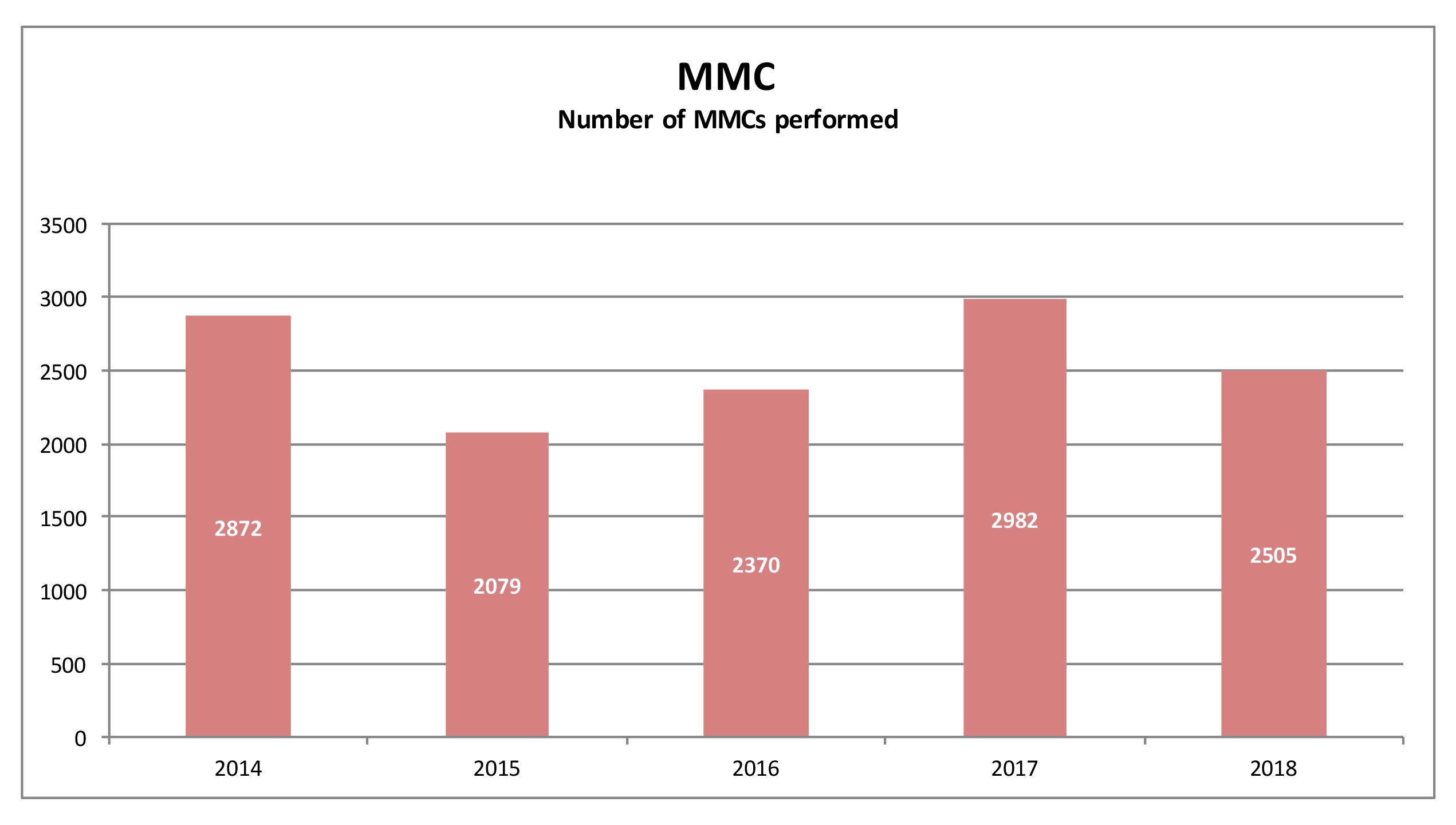
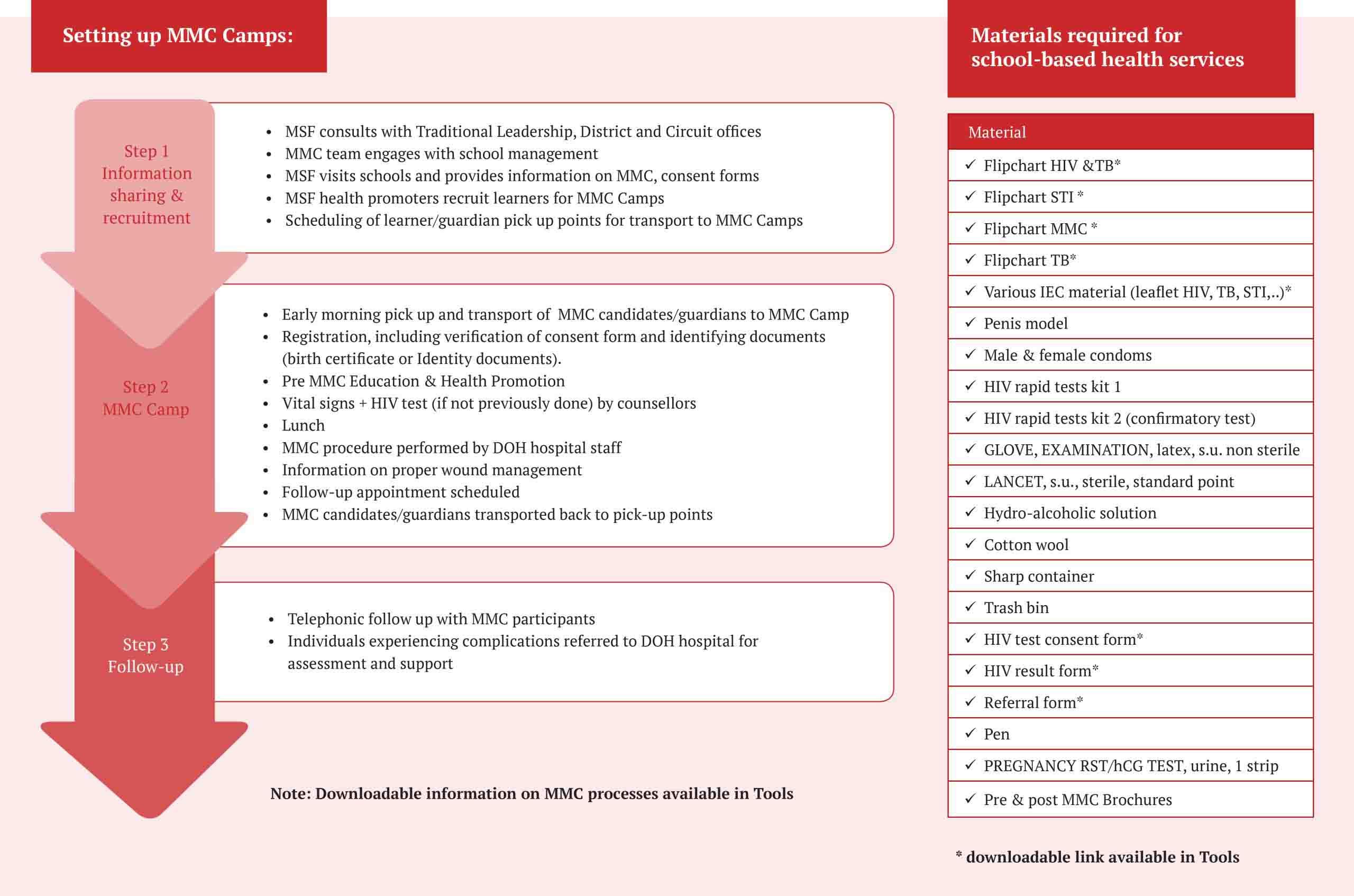
At the conclusion of each health education session male learners are presented with information about MMC. Parental consent forms are given to male learners who express an interest in receiving this service. Learners providing the required consent are invited to attend MMC camps run by the DoH. By end of September 2017, following MSF recruitment, just over 2,500 boys had been circumcised each year at DoH MMC camps.
Medical Male Circumcision - MMC
Training of Learner Support Agents (LSA) and Life Orientation Educators (LO)
In South Africa’s schools, LSAs and LOs are the role-players responsible for providing learners with support in relation to their health, as well as social, behavioural and poverty-related issues. They are therefore key role-players in any school health program, ideally ensuring that learners continue to receive access to information on sexual and reproductive health, as well as prompt referral to health services as required.
However, when MSF embarked on its School Health Program in 2012 LSAs were not present in most schools, and MSF staff quickly identified that not all learners were comfortable sharing their issues with LOs, as LOs are permanently employed, teachers. Additionally, many LOs said they did not feel adequately equipped to provide ongoing support to learners grappling with SRH issues.
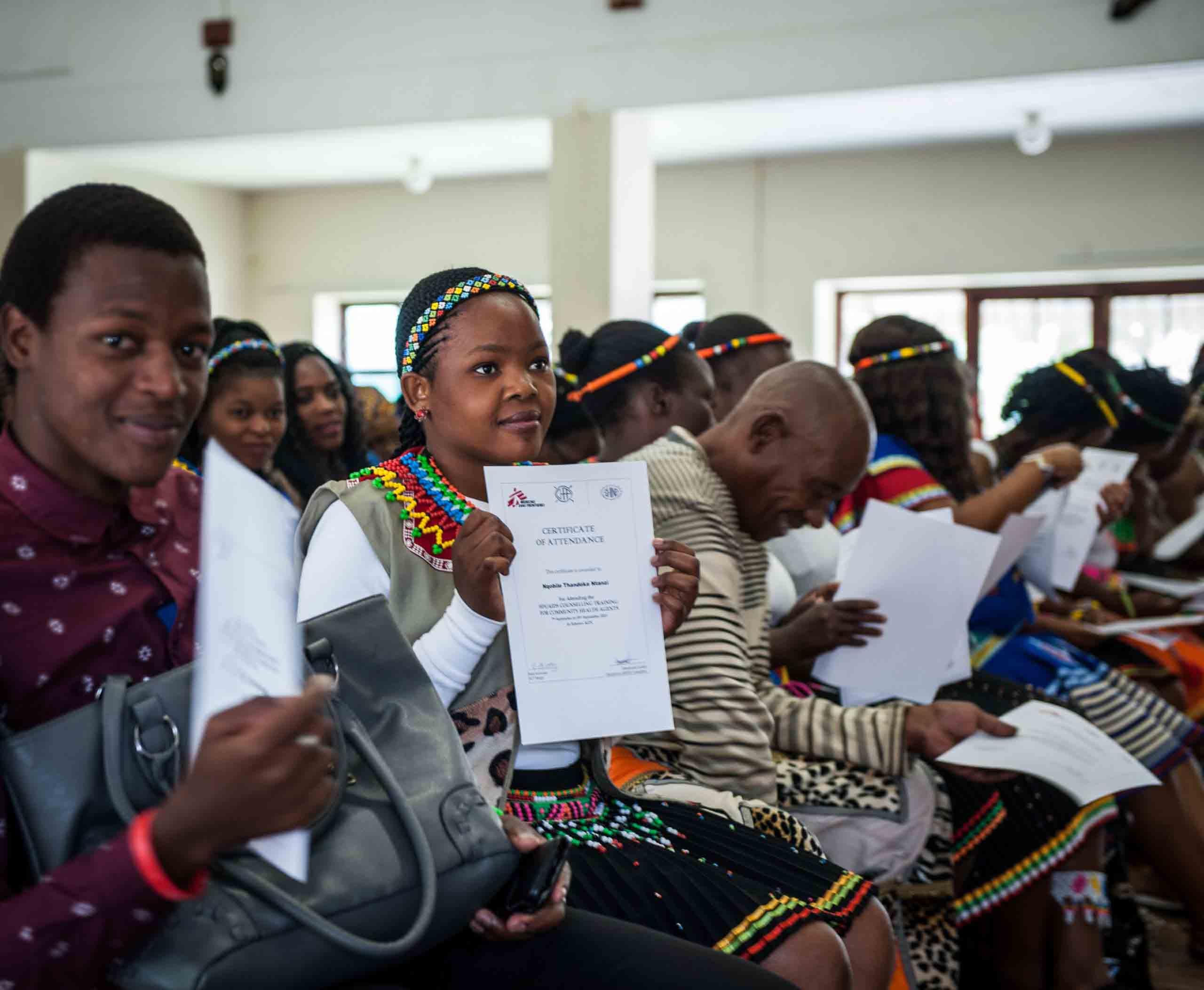
The DBE created the LSA role while MSF was implementing the School Health Program. LSAs are lay counsellors aged 18-35 who have been specifically trained to provide health support to school learners, including support on mental health and social issues. LSAs are employed by the DBE but are not permanent school staff, and MSF experience indicates that learners tend to feel more comfortable sharing intimate issues with LSAs.
However, the majority of secondary schools in South Africa lack the support of an LSA. MSF engaged the DoE in King Cetshwayo District on this issue and the result was the establishment of an MSF-led training program for LSAs and LOs, with a strong focus on HIV. Themes covered in LSA/LO training include:
- HIV/AIDS
- TB
- STIs
- Facilitation and counselling skills,
- Adherence to treatment and models of care
- Relevant laws and policies
Note: Downloadable LSA/LO training presentation available in Tools
MSF staff in partnership with the DBE have developed teaching manuals for both HIV and TB. The TB manual in the LSA/LO training is approved in terms of the DBE Curriculum Assessment Policy Statement. The HIV manual is aligned with DBE Curriculum Assessment Policy Statement.
Note: Downloadable HIV and TB training manuals available in Tools

Youth Camps
Since 2012, MSF has hosted an annual School Health Camp for select secondary school learners, in conjunction with the DoE and DoH. The initiative aims to develop selected learners as peer educators, and generates feedback that helps to keep the School Health Program dynamic and sensitive to the needs and preferences of learners.
Recruitment and Activities:
Two learners with leadership qualities from each participating school are invited by the school LSA or LO to join the Youth camps, totaling 80 - 100 attendees per Camp. Learners are accompanied by the school LSA and/or LO, and over the course of the weekend Learners and LSAs/LOs participate in a variety of health-focused activities during which health-related information is shared and relevant topics such as HIV/TB, disease prevention, and stigma are discussed. Insights are collected by MSF staff and this information feeds back into the design of School Health Program model.
Note: Example of Youth Camp Program available in Tools

Monitoring, Evaluation & Results
HIV Counselling and Testing (HCT)data capturing
HIV Counselling and Testing (HCT)data is uploaded daily to an open-source data capturing program called Kobo, using a smartphone, and this data is shared with the DoH on a monthly basis. HIV testing data is also recorded manually in an HTS Register and sent to the DoH on a weekly basis. Data is analyzed on a quarterly basis and indicators are presented in the MSF Quarterly Monitoring Report, which is shared with the DoH and local partners (example of Quarterly Monitoring Report available in Tools).
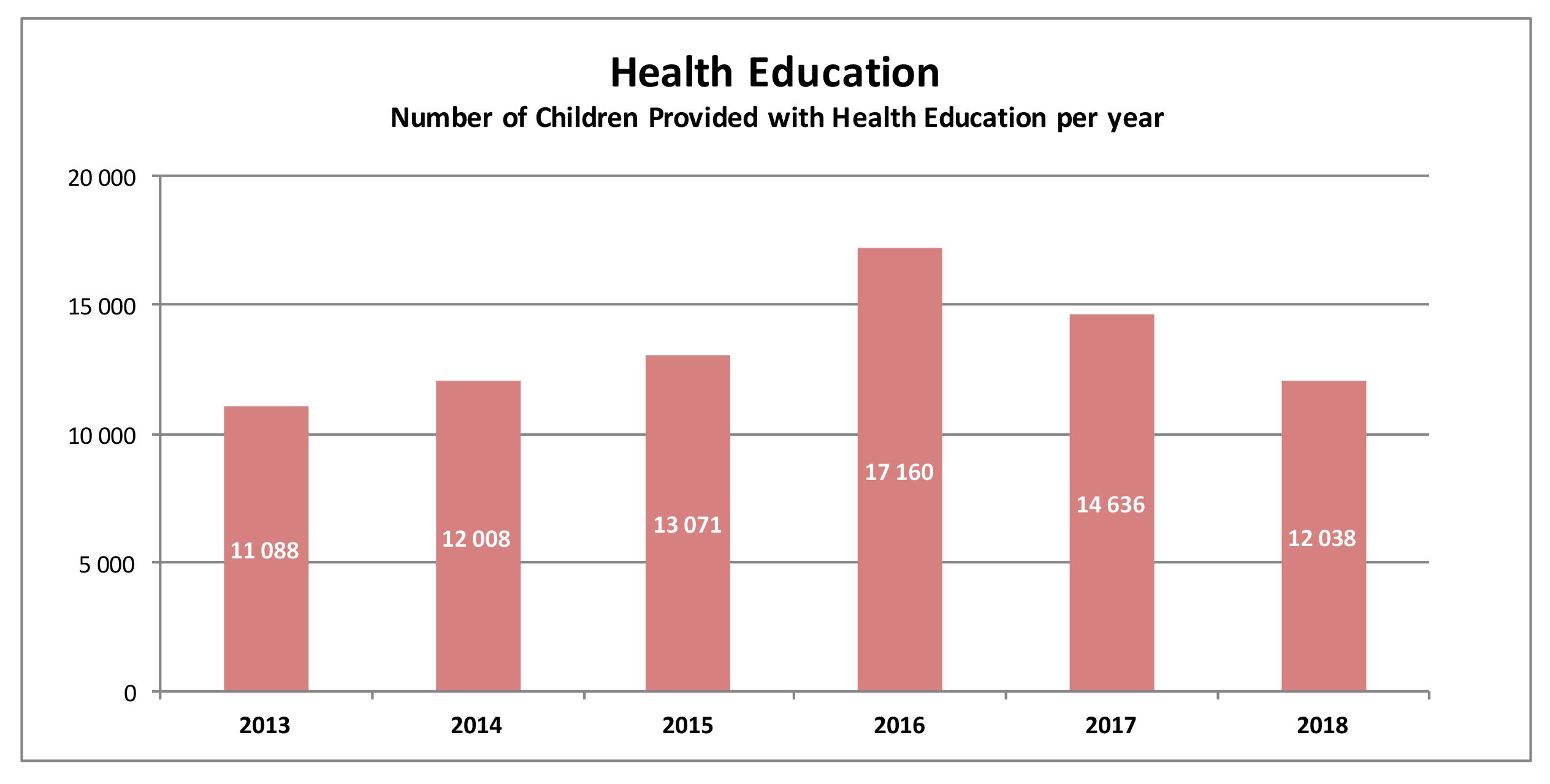
Data is also kept for Health Education Sessions, educator training and MMC. An annual report collates all quarterly program data and enables comparison with previous years.

Costs
Costing of School Health Program activities
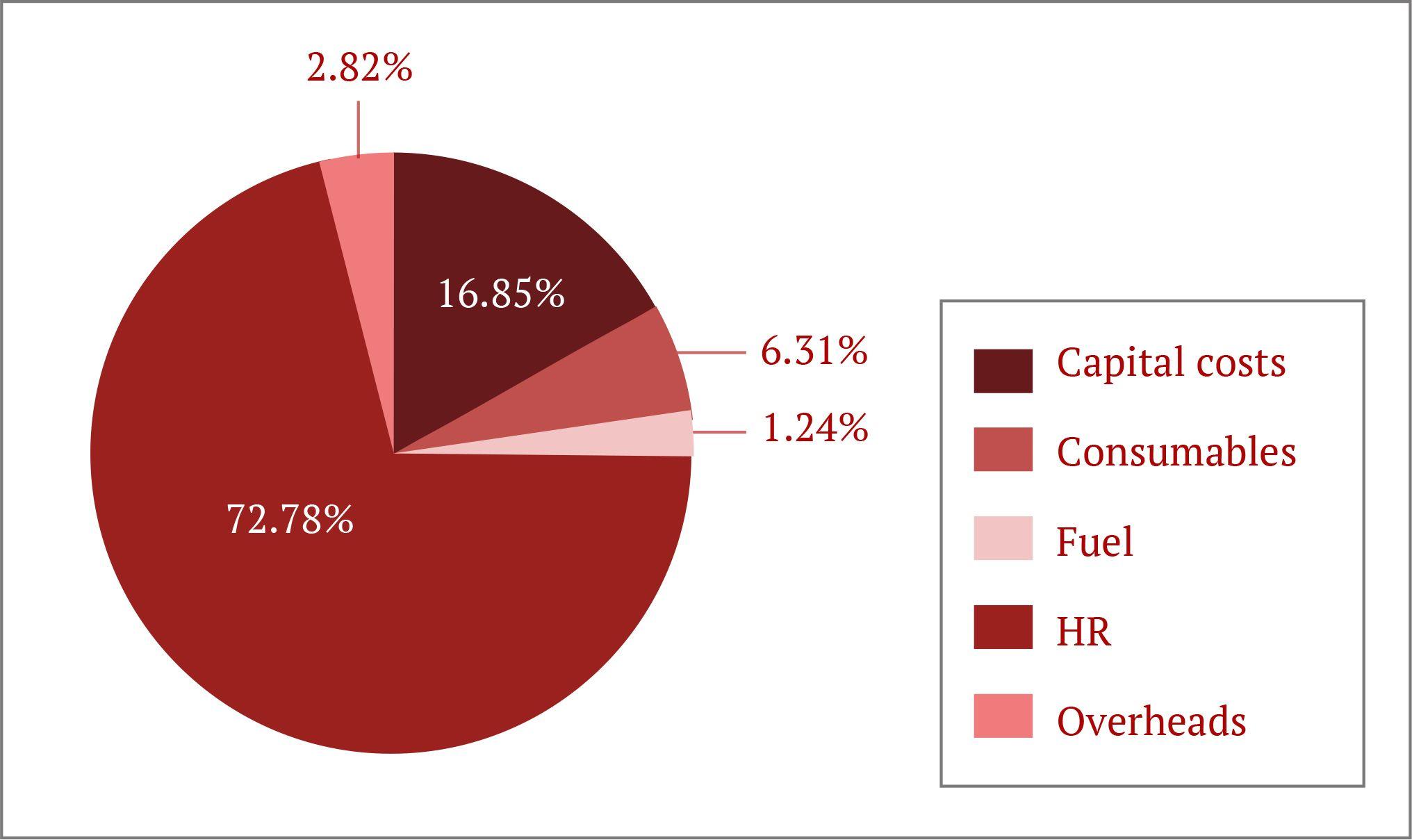
A costing of School Health Program activities was undertaken by MSF in 2017. Cost categories include fixed costs (equipment, furniture, buildings, and vehicles) and recurrent costs (personnel, consumables, fuel, medical supplies and overheads). Assumptions with regards to transport and staff allocation of time to the activity were informed by actual work practices.
The exercise revealed that Human Resources accounts for 73% of MSF spending on the School Program, although this does not factor in consumables and medical supplies, which are supplied by the DoH via the clinic nearest to each school, as per an agreement between MSF and the DoH.
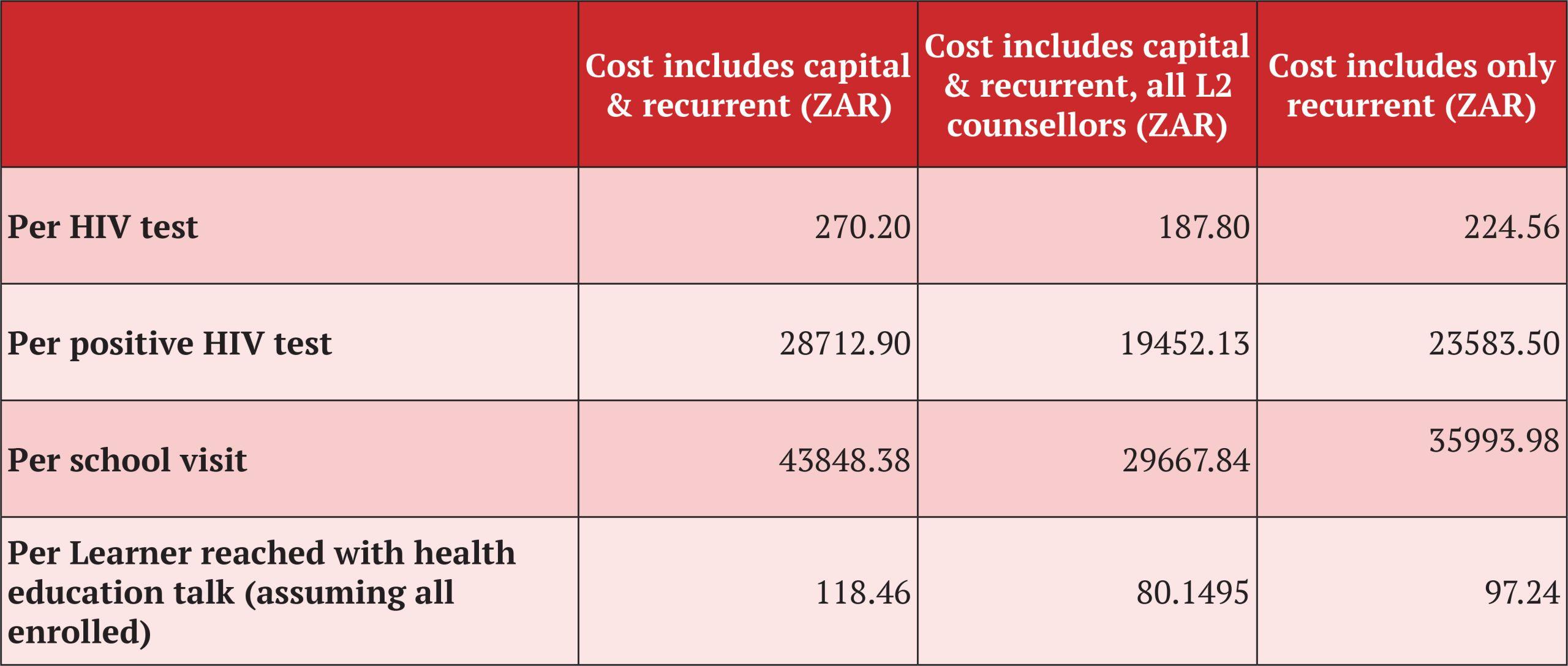
Additional notes:
MSF provides school-based health services from a mobile health van. The purchase cost of the van was included in the costing of School Health Program activities, as a mobile health van is not a requirement for providing school-based health services. DBE implementation guidance stipulates that school-based health services be provided in 'a room or designated area that is well-ventilated, learner-friendly and provides privacy to ensure confidentiality' [Section 4.2 DOB SOPs]

Challenges & Solutions
The MSF school program adheres to DBE policy and implementation guidance in regard to consent to receive school-based health services.
Challenge: Getting Consent
The MSF school program adheres to DBE policy and implementation guidance in regard to consent to receive school-based health services. However, MSF records indicate that fewer than 50% of learners who say they want to test actually return with a signed consent form. MSF is also aware of concerns in some schools that some learners sign the parent consent forms themselves.
SOLUTION 1: The DBE has developed a general consent form (see DBE SOPs), covering all annual activities requiring the consent of a parent/guardian. DBE could insist that this form be completed by parents as part of the registration process at the beginning of each year.
SOLUTION 2: Before parents are given the general consent form to fill out, the Provider of school-based health services could request a slot during start-of-year school parents meetings, during which the school health program and the importance of HCT and other SRH services to learner health are explained in detail, highlighting that parental consent is required before learners can access SRH services.

Challenge: Responsible disclosure
South Africa’s legal and policy framework for HIV testing requires that providers of school-based HIV Counselling and Testing (HCT) obtain the consent of both learner and parent, provide counselling and maintain confidentiality. Implementing these norms is not simple, and some of the most difficult challenges arise in relation to the disclosure of learner HIV status. Accidental or inappropriate disclosure to learners who are unaware of their HIV status can expose the learner and his/her family to negative impacts and could undermine trust in the School Health Program.
SOLUTION 1: Better alignment of HCT laws and policies will help to limit the scope for harmful misunderstandings in relation to HCT provision. Ongoing advocacy efforts are required to achieve this.
SOLUTION 2: Providers of HCT require training that covers the legal and policy framework around the provision of SRH services to adolescents; existing guidance on disclosing to adolescents; as well as thorough orientation in ethical issues concerning disclosures of HIV diagnoses to perinatally infected children and adolescents.

Challenge: Ongoing psychosocial support for learner with HIV positive status
It is difficult for learners to accept their status, as stigma remains very high in schools. Additionally, medical follow up and drug supply may result in absenteeism, causing the learner to fall behind. Ongoing psychosocial support is required and is in fact a DBE requirement for the provision of school-based SRH services. Providers of school-based services are only present for a few days a year, and it is, therefore, DBE roleplayers – principally the LSAs and LOs - who are best placed to provide ongoing psychosocial support. Learners are generally more comfortable confiding in LSAs, who are generally younger than LOs and they are not permanent staff members. However, there are not enough LSAs to support all secondary schools.
SOLUTION: The DBE should ensure that funding is available for at least one LSA per school

Challenge: Too little time for education sessions
The 45 minutes per class made available for health education sessions (occupying existing LO classes) currently does not provide enough time to complete the curriculum and address all learner questions.
SOLUTION: Running health education session over 1 hour will allow adequate time for discussion of SRH topics. This needs to be negotiated with the school principal and the LO.
Challenge: Inadequate time allocation for provision of health service
Time allocated for health services such as HCT and TB/STI/Pregnancy screening is often insufficient for all learners to access services
SOLUTION 1: If time runs out the senior counsellor must approach the school principal and request a date on which the team can return to complete the job
SOLUTION 2: MSF is working with the DBE to train LSAs and/or LOs as HIV referents capable of offering HIV testing and other services to learners throughout the year.

Challenge: Policy confusion around access to contraception
According to the Children’s Act, Section 134: “No person may refuse to sell condoms to a child over the age of 12 years; or to provide a child over the age of 12 years with condoms on request where such condoms are provided free of charge.”
However, the DBEs Integrated Policy on HIV, TB and STIs says that access is dependent “on age of consent, inquiry and need”, with the policy defining “age of consent” as 16 years and older. The policy also says that learners will only be able to access condoms by asking “suitable persons”. The DBE SOPs advise that “condoms should not be offered routinely, but should be offered after a careful risk assessment”. Law and policy are at odds, yet it is universally acknowledged that condoms are the most cost-effective intervention for preventing transmission of HIV and STIs.
SOLUTION: Condoms should be made freely available in schools and the near environment (i.e. nearby shops), via condomtainers.
Sexual reproductive health: Accessing condoms in schools

Tools
Downloadable files
Contact

For Operational Feedback and Support, contact Ntombi Gcwensa, MSF Patient Support Manager in Eshowe, email: MSFOCB-eshowe-htc@brussels.msf.org
For media or page-related queries, contact: MSFOCB-Capetown-ComsOff@brussels.msf.org
KwaZulu Natal Project, 33 Main St, Eshowe 3815, KZN, South Africa
Acknowledgements
Our sincere gratitude goes to make the MSF School Health Program a successful reality. It is with the assistance from our partners that have been able to support 67,963 learners (grades 8 to12) in 38 schools from Eshowe and Mbongolwane health service area in uMlalazi Municipality, King Cetshwayo District, KwaZulu-Natal, with school-based Sexual and Reproductive Health services, including education sessions and HTS services.
Thanks to the KZN Department of Basic Education and especially the DoE in King Cetshwayo District, for introducing the School Health Program within the schools in their catchment area.
Thanks to the Department of Health of KwaZulu-Natal – in particular to the officers in the School Health Department. Further, we would like to thank the District Health Offices of King Cetshwayo and uMlalazi Municipality as well as their respective Traditional Authorities and all community members that were involved in supporting the Programme.
Finally, acknowledgement is due to all the school staff role-players who make the implementation of the School Health Program a possibility, in particular the LO teachers as well as LSAs who played an instrumental role in all the program.