17-year-old Charles,* from Mwenezi, a rural district in Masvingo province, south-east Zimbabwe, was born with HIV. His mother died when he was still very young. By the time he was 14, Charles had to walk long distances from Mwenezi to Mberengwa, a neighbouring district to collect his HIV medication at Musume clinic.
In Mwenezi, people living with HIV used to travel long distances, as far as 60 kilometres, to collect antiretroviral (ARV) medication from the nearest clinics. In extreme cases, patients had to walk for two days to collect their medication.

“We used to wake up early in the morning and leave home around six o’clock to go and collect medication. We would arrive around 1pm if we walked fast,” explained Charles.
Walking these long distances will soon be a thing of the past following the introduction of new community-led models of HIV care.
While mentoring nurses from the Ministry of Health and Child Care (MoHCC) in Mwenezi, Doctors Without Borders (MSF) staff noted that many patients were defaulting on treatment and not taking their medication consistently. Most were defaulting because of the long distances to their nearest clinic and because they could not cross some rivers during the rainy season. MSF also noted that many young people in Mwenezi migrate to neighbouring South Africa in search of employment, causing them to default on treatment while away and coming back very sick.
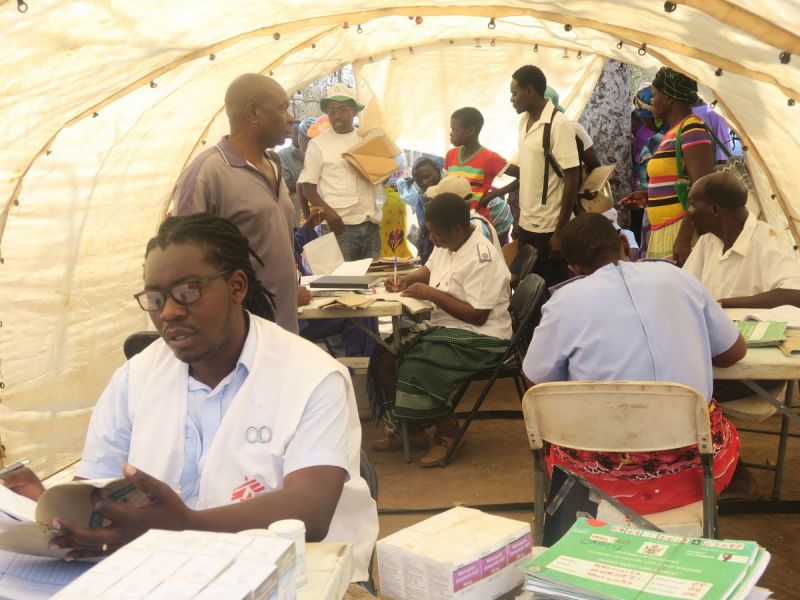
This prompted MSF to introduce an outreach programme in partnership with the MoHCC where MSF teams visited over 1,200 outreach patients in hard to reach areas and provided antiretroviral treatment (ART) and general outpatient department treatment.

Charles is happy that MSF has introduced an outreach programme as it means he can collect his medication at an outreach point rather than the main clinic which is too far away. Although the distance from their home to the outreach point is still far, it is much more manageable; a three-hour walk rather than a seven-hour one.
“I benefitted a lot from the services because I was sick but I have recovered now. I had chest problems and stomach pains, but I am feeling much better. I feel that I am healthier now,” said Charles.
Outreach programmes
MSF outreach teams travel distances of almost 200 km to reach patients who need medication.
“In the early days of our outreach programme, we saw many late presenters; people who had taken a very long time to get treatment after contracting HIV and whose HIV had progressed a lot,” said MSF doctor, Edson Chidovi.
“We saw patients who had been tested before, but had not begun their ART. They had been referred to the nearest clinic, which was 60 km away, and they had been forced not to collect their medication because of the distance.
Some patients had gone to collect their ARVs a few times, but because they had to cross major rivers that become impassable during the rainy season from October to March, they could not collect their medication for half the year. These are the people we are helping with our outreach programmes. Close to 40 percent of our clients presented with advanced HIV.”
Even with the outreach points, some patients were still travelling 40 to 60 km to collect their medication. After this realisation, MSF introduced new community-led ways for patients to get HIV treatment and care closer to their homes.
Some of the alternative models of care introduced by MSF in Mwenezi include community ART refill groups (CARGs), family refills, and out-of-facility community ART distribution (OFCAD). These models helped to improve patient access and adherence to treatment.
In the OFCAD model, village health workers are trained to distribute ARVs to registered people living with HIV in their communities. The village health workers collect ARVs from the nearest clinic and then keep them in their houses. People living with HIV are referred from clinics or outreach points to the village health workers facilitating OFCAD and can collect their ARVs from the village health workers approximately once every three months.
This is the first time that OFCAD is being piloted in Zimbabwe. It is also the first time it has been tried in a rural setting in the Southern African region. The concept has been used in Swaziland and the Democratic Republic of Congo, but in both cases it was implemented in urban settings.

Criteria for joining OFCAD
“For patients to be included in OFCAD, there is a criteria that has to be followed,” explains MSF nurse mentor, Tinashe Mbirimi. “Patients wishing to join OFCAD should have been on ART for at least six months, and their viral load should be below 1,000 or undetectable. They should be taking the fixed-dose regimen, which is Tenolum E. There needs to be a village health worker near the area where they are staying.”
Advantages of OFCAD
The advantage of using OFCAD is that people living with HIV can collect medication closer to home, saving them money and time, and greatly reducing the chance of defaulting from treatment.
“Community members will benefit from collecting their medication from the village. Before, they were facing many challenges,” said Rinet Zhou, a village health worker responsible for dispensing ARVs. “There are many rivers around and sometimes people are not able to cross them. In some rivers there are crocodiles. If the river is full, people can die while the pills are here.”
“Introducing OFCAD is a good initiative because we noticed that people were stressed just thinking that the day to go and refill their medication was approaching. Some live alone or are old, and collecting medication presented them with challenges,” said Rinet.

Other models of HIV care
CARGs are an established model of care that allow stable HIV patients on ART to form community groups. Group members take turns attending the health facility to pick up ARVs for the whole group. The system means that members spend less time at the clinic collecting their medication. Similarly, family refill is where one person can collect ARVs for other members of their family. The family refill is beneficial to people who migrate to neighbouring countries in search of employment but often come back home.
MSF started the Mwenezi HIV/TB project in March 2016. The project mainly focused on providing treatment and care for HIV and drug-resistant tuberculosis (DR-TB) patients.
The introduction of differentiated models of care, like OFCAD, presents potentially sustainable solutions for hard to reach areas like Mwenezi. The model can be replicated around Zimbabwe where there are similar needs. MSF is in the final phase of demonstrating that the OFCAD model is feasible and will soon call for its national implementation.
*Not real name
MSF nurse mentor, Tinashe Mbirimi shares how the greatest impact they made in Mwenezi was reaching the people and providing the services that they require here.
Find out more about MSF's work in Zimbabwe.
