

Zimbabwe
Doctors Without Borders (MSF) supported the Zimbabwean Ministry of Health and Child Care’s response to cholera with a range of activities, comprising treatment, donations of medical supplies, infection prevention and control measures, logistics, water and sanitation activities, and awareness-raising sessions in both urban and rural areas.
We had teams working in Harare, Epworth, Mazowe, Mbare, Hwange, Shamva, Kadoma, Kariba, Sanyati, and Chitungwiza. The outbreak lasted for 18 months, and affected people across 10 provinces.
Featured
Our activities in Zimbabwe in 2024
Data and information from the International Activity Report 2024.
98
98
€4.9 M
4.9M
2000
2
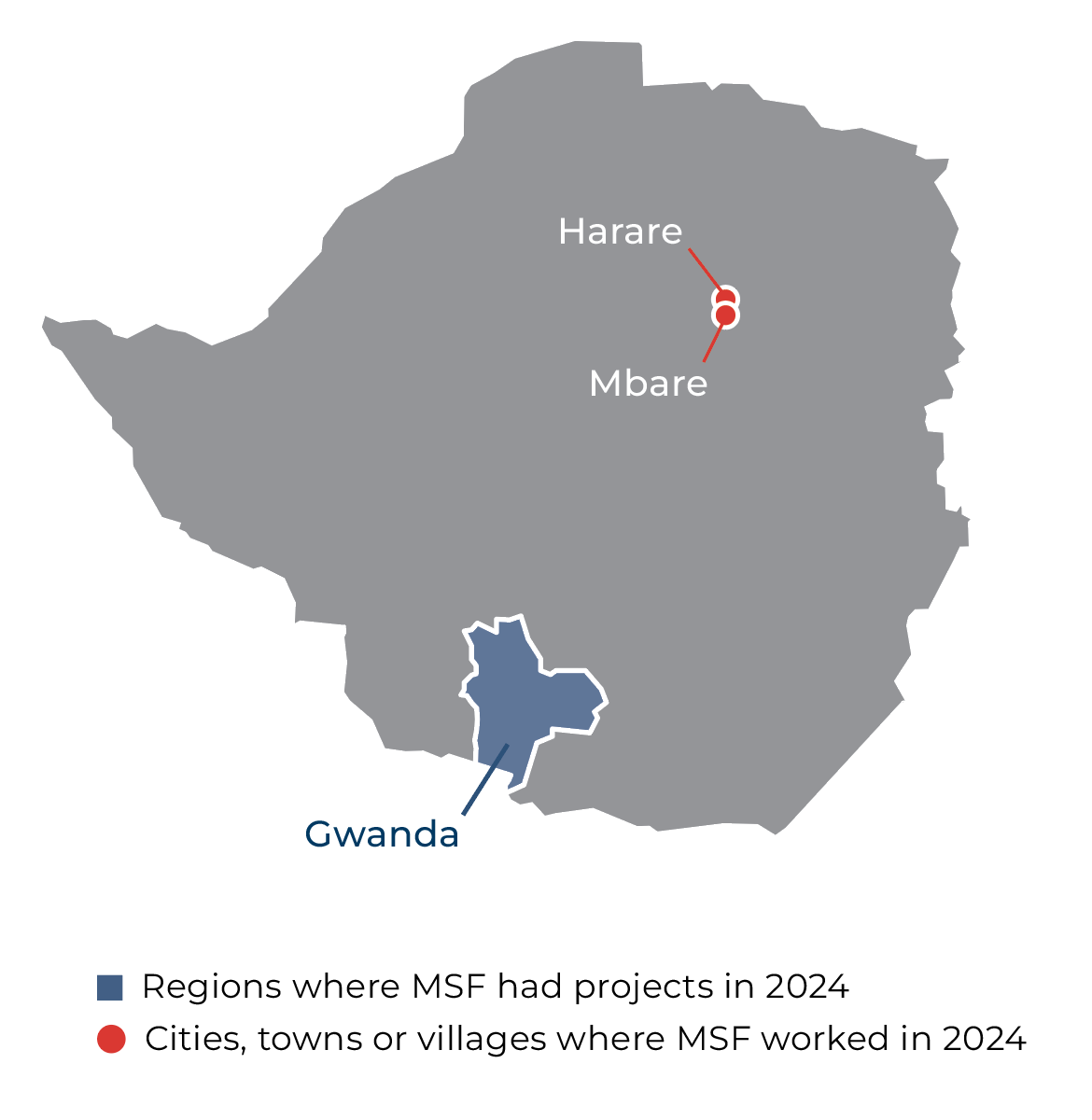
In Harare, we continued to offer comprehensive sexual and reproductive healthcare for adolescents and young people in Mbare and Epworth. Our services included mental health support, testing, treatment and counselling for HIV and sexually transmitted infections (STIs), family planning, and ante- and postnatal consultations.
To encourage participation in decision-making and to ensure that our services align with adolescents’ and communities’ health needs and realities, MSF established an adolescent advisory board. We set up a variety of communication channels, such as suggestion boxes in all healthcare facilities, WhatsApp and SMS messaging, and peer consultations, to strengthen patient feedback systems. We also launched community campaigns to raise awareness of patient rights, and conducted satisfaction surveys to gather critical insights into patient experiences and gaps in services.
In Gwanda district, Matabeleland South, we ran mobile clinics to serve small-scale artisanal miners and their communities. Due to rigorous screening and treatment efforts, we saw a reduction in STIs among the miners in 2024. We also screened miners for silicosis and tuberculosis, and all eligible women around the mines for cervical cancer.
In addition, we provided family planning services to the mining community, which included introducing a more effective injectable contraceptive method called Sayana Press. We also collaborated with the Ministry of Health and Child Care in mass drug administration campaigns for lymphatic filariasis, the provision of a variety of basic health services, and paediatric vaccination programmes.
IN 2024

2,710
2,71
280
28
28,200
28,2
230
23


Father first, miner Second: Why a Gwanda artisanal miner puts family before all

ZIMBABWE ANNUAL REPORT 2024
Treat the Funding Cuts like the Humanitarian Disaster that they are

A Day in the Life of an Epidemiologist in Zimbabwe

