Outsiders seldom get the attention they deserve. When it comes to conservation, for example, a few popular species attract most of the available funding – the rhino overshadows riverine rabbit. In the arts, jazz and blues struggle to attract the attention given freely to catchy pop, and it’s rare to see a documentary, however deserving, surpass the success of an action film at the box office.
It can be difficult to pinpoint why this sort of thing happens but the phenomenon extends to diseases too. A difficult and academic-sounding name does not help a disease gain widespread recognition. Some diseases mostly affect people living in low and middle-income counties, leading pharmaceutical corporations to view them as unprofitable (often a misperception). As a result, money doesn’t flow into needed research and development for treatments, in turn hampering the engagement of the wider scientific community.
Cryptococcal meningitis, which fits all of the criteria above, is a notable disease outsider, despite being responsible for an estimated 180 000 deaths annually, mostly of people under the age of 40 living in sub-Saharan Africa.

The causative agent, the cryptococcus, is everywhere in the environment. For those of us with a fully functional immune system, it causes no harm. However, in people with HIV who have severe immunosuppression, it can invade the lining of the brain, quickly leading to severe disease and death if left untreated.
This grim picture may lead you to think that cryptococcal meningitis is incurable, but this isn’t the case. In fact, with early diagnosis and optimal treatment, mortality could be reduced by over 70%. Achieving this at the population level, by ensuring everyone with the disease was managed well, would help to avert hundreds of thousands of deaths between now and 2030.
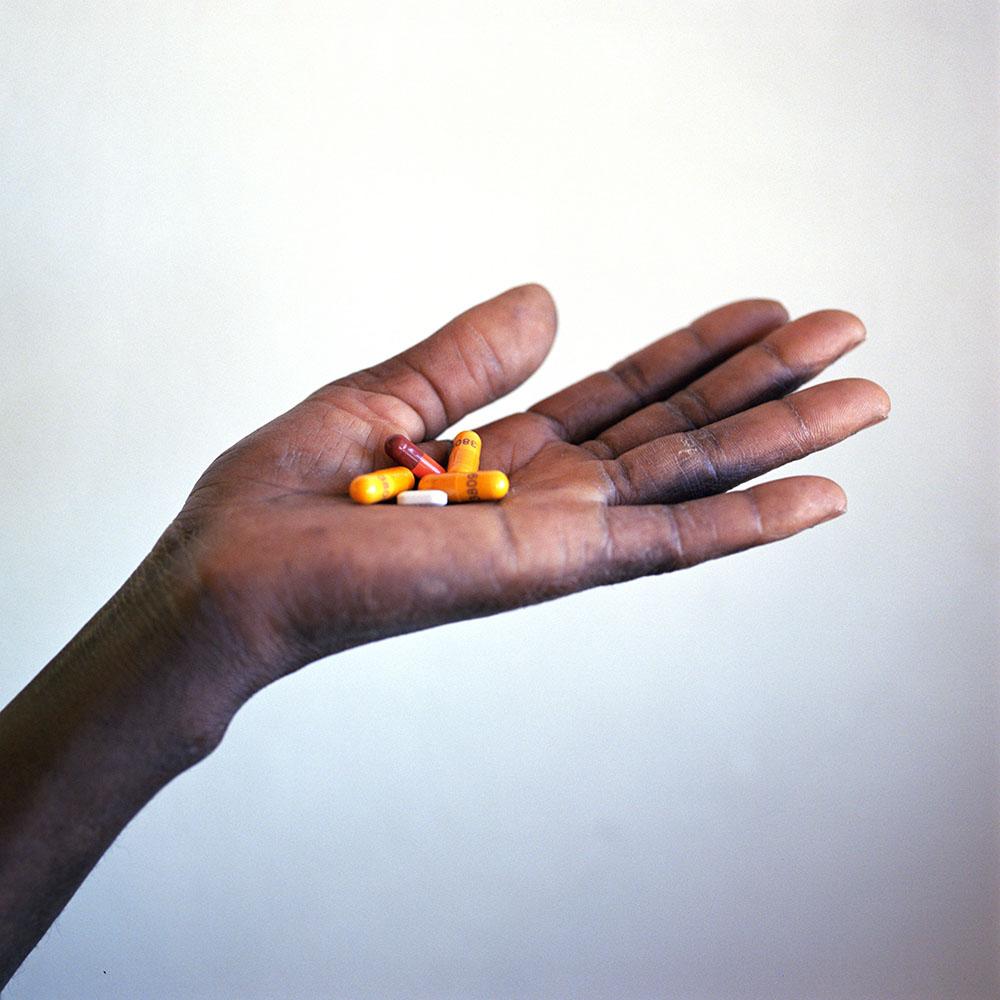
This is far from the current reality, and it is a marker of the lack of recognition given to this disease that life-saving tools developed decades ago are still barely used today. Flucytosine - an essential drug for the treatment of cryptococcal meningitis - was developed in the 50s, is off-patent and is very simple to make.

Yet, most people with the disease today will never access it. There are many reasons for this lack of access: funding challenges, low clinical awareness and a need for training. The other big reason why flucytosine is rarely used is the fact that it is not registered in most countries where it is needed. On World AIDS Day 2021, it is time for countries to address that.
In South Africa, for example, while registration has been in process under the South African Health Products Regulatory Authority (SAHPRA) for almost 2 years, it has still not been finalised. SAHPRA should urgently proceed to register this medicine, following which the government of South Africa has an opportunity to rapidly ensure all of its people who need it can access this life-saving medicine by rapidly rolling out supplies and necessary support.
Cryptococcal meningitis and the bigger HIV picture

Scaling up antiretroviral therapy is by some way the most important means of improving the lives of people living with HIV (PLHIV) and addressing the AIDS epidemic, but it is not by itself enough. In 2019, there were still 690,000 deaths from HIV-related causes, including opportunistic infections like cryptococcal meningitis. Improving things on the treatment side of the equation could help address that.
In HIV care, a public health approach and quality care for the very sick have for too long been pitched as mutually exclusive. It is time to focus proportionate energy and investment on PLHIV who become sick with opportunistic infections, ensuring that they get the care they deserve.
What needs to change?
There is a global strategy to end tuberculosis, the biggest killer of PLHIV, but no strategy to end cryptococcal meningitis, nor other major causes of death of PLHIV.
UNAIDS and the WHO, the multilateral health organisations at the helm of the HIV response, can help by acknowledging the seriousness of the problem through steps that include measuring cryptococcal meningitis deaths, setting targets for reducing those deaths, and helping countries develop strategies for meeting those targets.
It is regrettable when an outsider doesn’t receive due recognition. In the case of cryptococcal meningitis, it’s an avoidable tragedy.