Tinashe Mbirimi is a nurse mentor with Doctors Without Borders (MSF). He joined MSF in October 2008 under the Murambinda project in Buhera before transferring to Gutu in 2011 and Mwenezi in 2016.
“When we first came to Mwenezi, Zimbabwe in 2016, we were mentoring Ministry of Health and Child Care (MoHCC) nurses to provide antiretroviral treatment and care to patients with HIV and TB. While visiting clinics, we noted that many patients were not attending follow-up appointments and were not regularly taking their medication. When we tried to establish what was happening to these patients, we found that they were patients that were coming from hard to reach areas with no clinics nearby.
In September 2016, we started an outreach programme in Mwenezi, which proved very popular. There was a high volume of patients accessing the services and we were not able to manage all of them with the limited number of staff that were available.

Many of these patients had advanced HIV, some were defaulting and some were already failing on treatment. Treatment failure occurs when a patient is not responding well to treatment. Some of the patients were very ill with a lot of opportunistic infections; these are infections that often occur in people with weakened immune systems.
We would see 120 to 130 people a day. Due to the long distances we had to travel, sometimes we would only have four hours to work.
We decided to introduce community ART refill groups (CARGs) to decongest the outreach sites. CARGs are a new model of care that allow stable HIV patients, who are on ART, to form groups in the community. Group members rotate attending the health facility to pick up antiretroviral medications (ARVs) for the whole group.
However, even with the CARGs, we continued to see many patients at the clinics and people who were coming from other nearby districts like Mberengwa and they started to transfer to come to the outreach sites. Patients were continuing to arrive even when it was time for us to leave, some were coming from more than 40km away and it was also expensive and time consuming for them to travel.

We asked ourselves if there was anything else we could do to assist these patients. We decided to introduce a model of care called Out of Facility Community ART Distribution (OFCAD), which would address the sustainability of the programme.
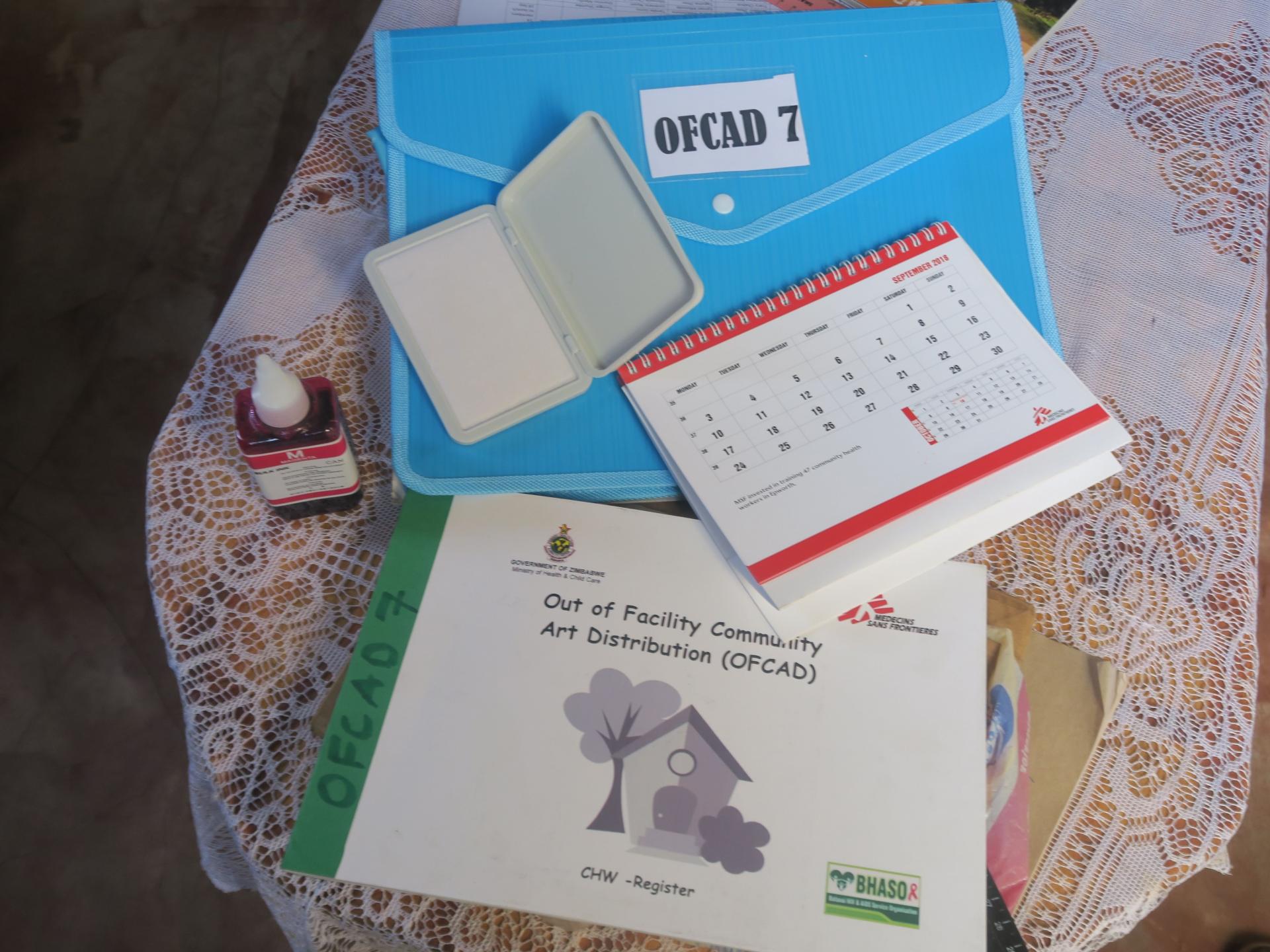
Through the OFCAD model, village health workers are trained by the Ministry of Health and our partner BHASO to distribute ARVs to registered people living with HIV in their communities. BHASO is a community-based organisation that mobilises people in the community.
Selected village health workers collect ARVs from their nearest clinic and keep them at their houses. People living with HIV are referred from clinics or outreach points to the village health workers facilitating OFCAD. In turn they are registered to collect their ARVs from the village health workers approximately once every three months. We are keeping the medication in the community, with the patients, to cut down distances and reduce travel costs.
For patients to be included in OFCAD, there is a criteria that has to be followed. Patients must be willing to join OFCAD, they need to have been on ART for at least six months, and their viral load should be below 1,000, or undetectable. They should be taking the fixed dose regimen, Tenolum E. There has to be a community village worker near where they live.

Village health workers attend meetings every month where they order more medication for the patients in their community. The drugs can be kept at a room temperature, in a well-aired room. MSF provides lockable trunks.
MSF conducted two training sessions, one for nursing staff and one for village health workers. We follow this with on-the-job training whenever we visit them. There is continuous mentoring. When they go for their monthly clinics, they also get training. We hope OFCAD will address sustainability issues so that communities continue to benefit from the services even after NGOs have left the area.
A day I will always remember was when we got stuck on one side of a river. We wanted to go for the medical outreach programme so we left early in the morning, around 6.30 am, but by midday we were stuck on the wrong side of a swollen river that we couldn’t cross.
We waited for almost two hours and were wondering what we were going to do about the 100 patients we were meant to see that day. We had to wait until about four o’clock before it was finally safer for us to cross. When we eventually managed to get to the outreach point our patients were still waiting for us. They had patience and confidence that we were coming to provide treatment. It was so touching. When we arrived, they were so happy. Some patients even cried. They could not hold back their tears. We had told them that we are MSF; whatever happens, we will come.

As a humanitarian worker, I was so happy and satisfied that, although we were late, we managed to finally arrive and provide healthcare services. Seeing patients recovering from illness makes my life worthwhile. When we are coming to the field, our work is patient centred. We ensure patients get well and improve their lives.
The biggest challenge in Mwenezi is that there is no safe drinking water. Villagers get their water from wells they drill on the river banks. People and animals sometimes get water from the same water source. There are also very few clinics in the area.
The general environment in Mwenezi is not very favourable, but what kept us going was the desire to see people benefiting from our services. I want to see these patients improving and getting the services they require. That is my motivation. I believe people here should get the same services as people in Harare.
The greatest impact we made is Mwenezi was reaching the people and providing the services that they require. We really improved their quality of life. They are now able to access treatment. Other NGOs are now also coming in and we are glad to have pioneered the process and shown them how it can be done.”
Find out more about MSF's activities in Zimbabwe