In 2014, Doctors Without Borders (MSF) began offering sexual and reproductive healthcare and HIV prevention and treatment services in Beira, Mozambique. After 11 years of collaboration with the Ministry of Health (MoH) and local organisations, MSF is now handing over its medical activities to its partners.
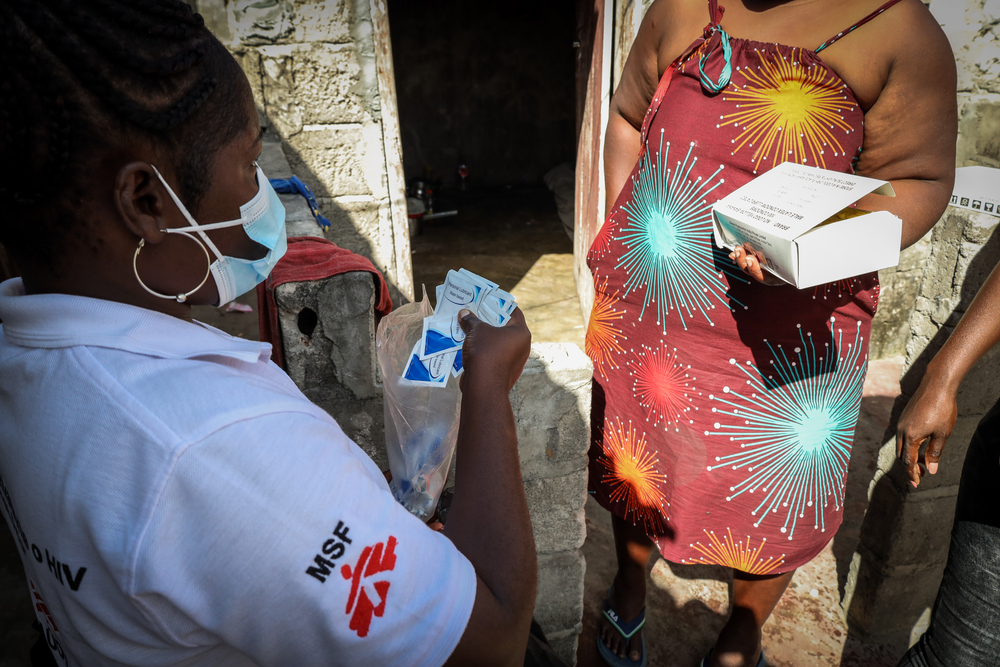
MSF work in Beira focused on providing tailored care for vulnerable and highly stigmatised groups who are at a greater risk of contracting HIV, including sex workers, adolescents, men who have sex with men, and transgender people.
Dr Zaid Seni, MSF deputy project coordinator, tells us more about the project’s highlights
Give us a brief overview of your work with MSF in Beira
I first joined the organisation six years ago as a medical doctor during the emergency response to Cyclone Idai. I later became the medical activity manager, focusing on interventions for key populations such as sex workers, men who have sex with men, transgender people, and truck drivers, as well as work around advanced HIV care in primary health facilities. I now serve as the deputy project coordinator.
The Beira project began as part of a multi-country initiative called the corridor project, which addressed the spread of HIV along the major transport/economic corridor between Mozambique, Zimbabwe, Malawi and South Africa. One of the elements leading to HIV spread in the region was related to sex work. However, because key populations often face stigma, including in health facilities, they struggled to access proper care. MSF tried to address this gap through a community-led approach, including door-to-door outreach, mobile clinics and, later, by providing support to MoH facilities.

Peer educators in Beira
How did the project evolve?
Over time, we started to understand the community’s needs, as well as those of the MoH and decided to expand our services. We began supporting the Beira Central Hospital, which receives patients from the entire central region. Our goal was to reduce mortality among people living with advanced HIV. We later included primary healthcare facilities and introduced innovative strategies like mentorship to build long-term capacity for MoH staff and to ensure sustainability. In 2022 and 2023, we also added interventions addressing antimicrobial resistance and healthcare services for survivors of violence among young people.
What was unique about MSF’s approach?
We used a ground-up approach rather than a top-down one, looking to people to provide data when developing a public health-related strategy. We already had information on the prevalence or incidence of HIV and sexually transmitted illnesses, but we did not want to impose a framework of our services on the community. What we needed was to understand the context, the daily routines of our target group and to hear them expressing these issues in their own words. We then used the community feedback to create a model of intervention that was more suited and relevant to them.
We listened to the community, hired people from key populations and developed strategies together to tackle their specific needs. This collaborative model allowed us to respond to real needs and created an environment where healthcare workers like me learnt directly from the people we served. This was a true community-led intervention, with MSF providing the resources needed to realise the community’s priorities.
It’s important that MSF does not stay for too long as our goal is to fill urgent gaps, introduce effective models, and leave once local structures can continue the work.Dr Zaid Seni, MSF deputy project coordinator

Why was building strong community relationships important?
Creating relationships was critical, especially because we wanted to implement something very specific and offer specialised services. When we started our intervention, there was an existing structure; community-based organisations, the Ministry of Health, community leaders, international organisations and other partners already providing services in the community. We wanted to be known and to also know the community well. So, it was good for us to provide door-to-door services, inviting the community to help shape the intervention and to bolster our identity here. Little by little, we started gaining acceptance and our relationship with all these partners became stronger because they saw value in our project.
How did MSF support community-based organisations like Takaezana?
Supporting community organisations has been one of the most exciting parts of the project. Takaezana, a peer-led organisation created by former MSF peer workers, is now able to run its own interventions and secure its own funding.
We helped them build technical skills, manage programmes, and strengthen networks. They have become an important partner in delivering services to key populations and even participate in operational research, an area where Mozambique needs more capacity. Their growth is a strong example of sustainability in action that we are proud of.

How did MSF ensure the sustainability of the project?
We identified three major challenges in achieving sustainability: 1) instability in the national health system, particularly in the supply chain, 2) structural stigma, including among healthcare workers and 3) low engagement with healthcare services among key populations. To address these, we strengthened the MoH supply systems and communication and provided on-the-job training, coaching and mentorship to healthcare workers to try and mitigate stigma and encourage a patient-centred approach in healthcare facilities. Other initiatives included the creation of focal points for key populations in health facilities so that people felt comfortable requesting services, and we introduced MoH teams to communities to reduce stigma. This multi-layered approach helped ensure that services would continue effectively after the handover.
What are some of your memorable moments?
A particularly powerful memory comes from my time working as a volunteer doctor at Beira Central Hospital before I joined MSF. At that time, patients with cryptococcal meningitis were often sent home with only painkillers because more effective treatment wasn’t available. I remember a 32-year-old woman who died because we could not treat her. At the time all I could prescribe to her was paracetamol and a few antibiotics.
Later, when I joined MSF and learnt that this disease is treatable with existing resources, it felt like a light at the end of a tunnel. Today, thanks to MSF’s work and advocacy, the MoH can treat such cases more effectively. Knowing that future doctors won’t have to send patients home to die is one of the project’s greatest achievements.
Why can’t MSF just continue working in Beira?
It’s important that MSF does not stay for too long as our goal is to fill urgent gaps, introduce effective models, and leave once local structures can continue the work. We started a wheel of intervention here and it is working, so the MoH can now take over. For long-term success, the Ministry must lead