Dakar/Brussels - As African heads of state meet today in Addis Ababa to endorse the Emergency catch-up plan led by UNAIDS to accelerate HIV treatment in West and Central Africa, the international humanitarian medical organisation Doctors Without Borders (MSF) reiterates its call for a clear roadmap and strong political commitment from affected governments and all international stakeholders, towards removing longstanding barriers and implementing proven simplified strategies that will boost lifesaving treatment for 4.7 million living with HIV not yet accessing antiretroviral therapy (ART).
Lower rates of HIV prevalence in the region’s 21 countries, ranging from 2-10%, have long resulted in less attention and investment in its overall HIV response. Here, only 28% of people and 20% of children living with HIV have access to ART, resulting in high numbers of deaths and an incidence outpacing treatment initiations.
Faced with these obstacles, staff in MSF-supported HIV hospital centres in Conakry, Guinea, and Kinshasa, DRC report that in the last quarter of 2016, patients arrived in such advanced stages of HIV that 43% and 36% of them respectively died during admission and around third of these died within 48 hours of admission.

Today’s meeting is aimed at deepening engagement from governments, key policy makers and donors towards the implementation of a regional emergency HIV plan and furthering country-specific acceleration plans in fourteen priority countries to start. MSF strongly commends the vital leadership shown by UNAIDS and African states in initiating the Acceleration Plan.
African leaders are urged to address any limiting factors which may prevent its full realisation. These include legal and policy blockages, centralised health systems, weak procurement and supply chain management, financial barriers including user fees for patients, and high levels of stigma. MSF also asks for the Acceleration Plan to soon include remaining countries in the region that face similar treatment gaps.
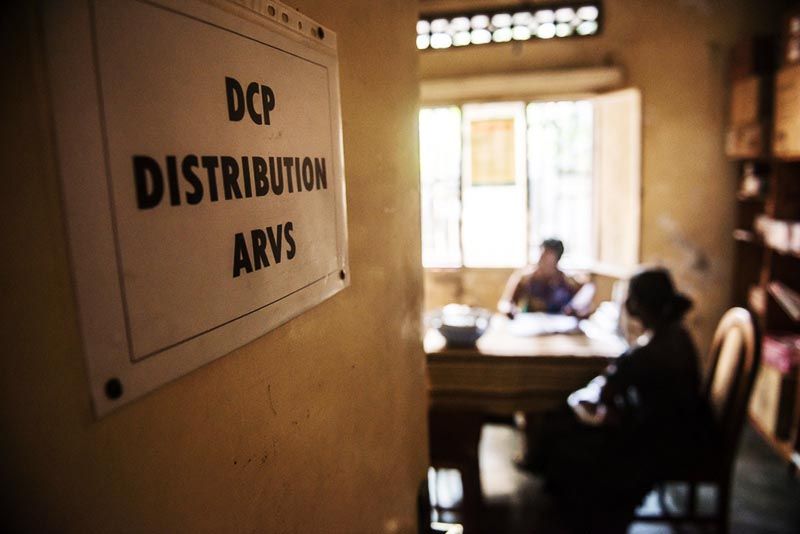
“This is a pivotal opportunity to anchor governments’ efforts in clearly defined and inclusive country action plans that tackle the many obstacles that people living with HIV face every day. Each patient presenting with late stage AIDS in our hospitals is a terrible testimony to these challenges. Our patients tell us often of unimaginable suffering simply trying to access diagnosis and treatment: empty shelves, insurmountable fees and transport costs, long queues, and stigma and discrimination in health facilities,” said Joanne Liu, MSF International President.
Key strategies central to the HIV response in southern and eastern Africa during the 2000s would strongly support a wider response based on quality care for patients. Along with other organisations, MSF calls for the elimination of user fees that would enable a move to ‘test & start’ (immediate treatment on diagnosis) and keep people healthy on lifelong treatment.
Improvements in supply management and last mile delivery should also include strong monitoring mechanisms of stock outs by civil society and patient organisation.
Reaching wider numbers will require the implementation of ‘task-shifting’, where basic tasks are delegated to nurses and lay health workers to carry out tests, prescribe and dispense ARVs, counsel patients, and contact defaulters.
These so-called ‘differentiated models of care’ have been successfully piloted by MSF in Kinshasa, DRC, and Zemio, Central African Republic, allowing the decentralisation of simplified HIV service delivery models to the health facility and community levels.
The role played by civil society and patient associations in the HIV response is essential. MSF witnesses the reluctance of health ministries and governments and international implementing partners to fully include civil society and communities service delivery, testing and adherence support, as well as stigma reduction activities and service monitoring.
The ‘community treatment observatories’ now running in Burkina Faso, Cameroon and DRC are strong examples of this watchdog function. These valuable entities require steady funding and technical support and should be scaled up in all countries in the region.
“West Africa, civil society, and communities of people living with HIV groups remain isolated and underfunded, with little support from international civil society, governments, and donors. In Eastern and Southern Africa, engaging people living with HIV in the responses contributed to vigorous achievements overall in increasing antiretroviral coverage, support, and care. We need to invigorate treatment literacy which gives people autonomy over their care and addressing stigmatising attitudes.” said Amanda Banda, MSF’s HIV Advocacy Coordinator.
“In Eastern and Southern Africa, engaging people living with HIV in the responses contributed to vigorous achievements overall in increasing antiretroviral coverage, support and care. We need to invigorate treatment literacy, which gives people autonomy over their care, and address stigmatising attitudes.”
*Benin, Burkina Faso, CAR, Cameroon, DRC, Gabon, Guinea, Côte d'Ivoire, Liberia, Nigeria, Chad, Togo, Senegal and Sierra Leone (UNAIDS).
MSF currently supports treatment for over 200,000 patients in 19 countries, primarily in Africa. This includes HIV programs and activities in West and Central Africa: DRC, Guinea, CAR, Chad, Niger, Mali as well as other countries with low ART coverage such as South Sudan, Yemen, and Myanmar.
