People who use drugs are among the most vulnerable groups of people and are exposed to a range of severe health conditions. Yet, they are also among those with the least access to prevention, care and treatment services as a result of widespread stigma, discrimination and harassment, often related to the criminalisation of drug use.
In Mozambique, people who use drugs often fear being arrested for carrying drug paraphernalia and end up sharing or even hiring needles to inject drugs.
To provide them with much needed medical and preventive care, MSF joined forces with UNIDOS, a local community-based organisation working with people who use drugs, to start harm reduction services in the informal settlement of Mafalala, Maputo.
What is harm reduction?
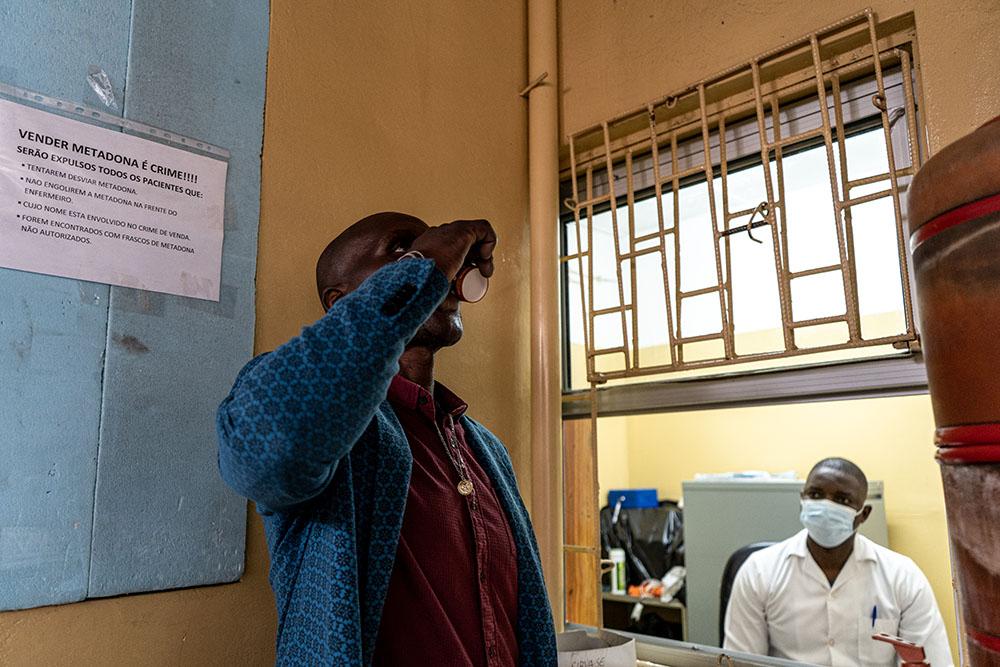
Harm reduction is a set of policies, programmes, services and actions that aim to reduce the harm caused by drug usage. This includes a needle exchange programme, opioid substitution therapy (using methadone) and overdose treatment (using naloxone). Harm reduction programmes are recommended by international health bodies WHO, UNAIDS and UNODC as they reduce the harms related to injecting drug use and have proven to reduce the spread of HIV and viral hepatitis among people injecting drugs.
Providing medical care for people who use drugs is an important measure in the fight against HIV, Hepatitis C and other blood-borne diseases in Mozambique. Mozambique has one of the highest HIV infection rates in the world (13,8% of the population) and it is particularly high among people who use drugs. 41% of drug injectors coming to MSF for care tested positive for HIV, and 27% tested positive for viral hepatitis. Preventing the spread of blood-borne disease among people who use drugs serves the whole community, as it reduces exposure.
Tea, safe injection kits and HIV testing – Specific services for specific needs
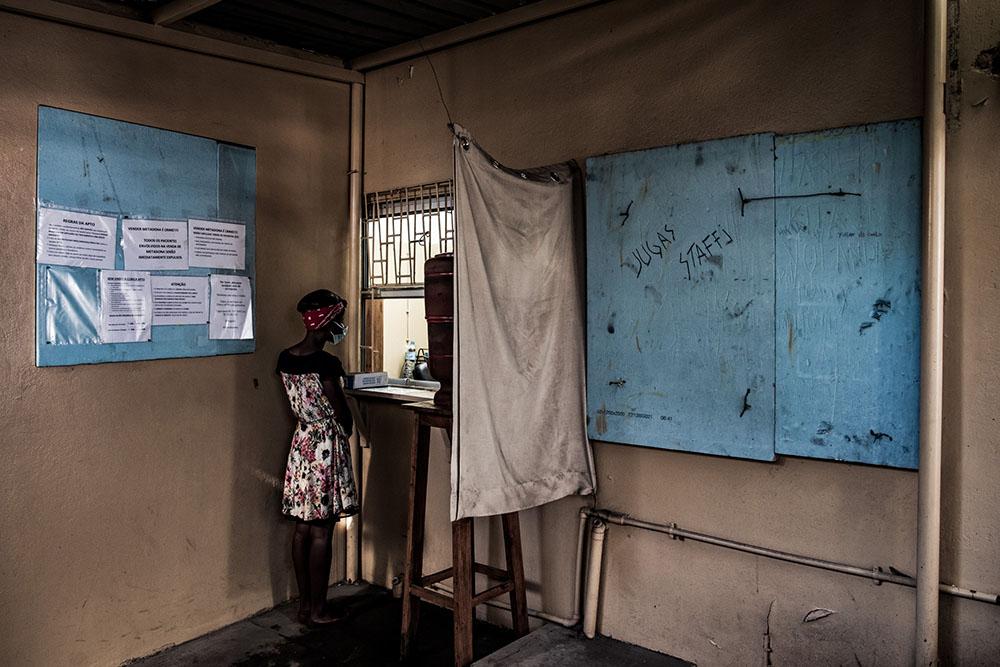
People who use drugs often avoid seeking healthcare. MSF and UNIDOS, therefore, decided to offer services that catered for their very specific needs. The Centro Comunitario para Pessoas que Usam Drogas thus opened its doors in May 2018. This drop-in centre is the first point of contact for health services for people who use drugs.
It provides testing for HIV and other illnesses and ensures those who need it receive medical care for conditions including HIV, hepatitis B and C, TB and sexually transmitted diseases. People who come to the centre can receive counselling, psychosocial support and can have minor injuries treated by trained nurses. For many, the centre provides a safe, stress-free environment where they can have a shower, wash their clothes, rest and relax with a cup of tea.
To reach people who use drugs, MSF/UNIDOS teams work alongside peer workers (made up of former or current people who use drugs) at the hotspots, where heroin is consumed. There, they talk to people about safe injection practices and sexual behaviour, and the services available in the drop-in centre. They also offer HIV and hepatitis C testing and distribute and collect syringes. This outreach approach allows them greater access to people who use drugs, including those who otherwise may not visit regular health centres or even the drop-in centre.
Opioid overdose is one of the leading causes of death among people who inject drugs worldwide. Many people coming to the Mafalala drop-in centre told MSF about friends who had died from probable overdoses. In response, MSF has trained community members to recognise an overdose and how to administer Naloxone, a lifesaving medicine that is used to reverse the effects of opioids.
A project by the community for the community
The nature of the drop-in centre’s activities was new for the local community. As such, it was important to involve them from the very beginning in how to run the project to ensure it was accepted and understood. A steering committee, made up of formal and informal community leaders, influential people in the slum and, importantly, people who use drugs, was created to help guide the management of the drop-in centre and represent the community’s perspective. The committee helps to address concerns, relay recommendations and promote public understanding of harm reduction activities.
We are humans too: A story of how harm reduction is giving people who use drugs hope in Mozambique.

Addressing essential health needs
The Mafalala project was the first to pilot a full harm reduction programme in Mozambique. The combination of harm reduction and health services constituted a completely new model of care, based entirely on the needs of the people using the services. The MSF/UNIDOS pilot project in Mafalala showed that it is feasible to address the needs of people who use drugs and implement effective harm reduction activities in a resource-limited setting.
The results of its activities have demonstrated significant potential public health benefits. Protecting people who use drugs from harm and providing them with care not only addresses their needs but is also essential to combat the spread of HIV, hepatitis C and other bloodborne diseases.



