

Kenya
Our teams continued to deliver healthcare in Dadaab, a huge, overcrowded camp complex, which currently hosts more than 350,000 refugees.
During the year, we repeatedly called for better living conditions and increased humanitarian assistance for the constantly growing population, especially in Dagahaley camp. In Kiambu county, we supported refugees who had fled Kakuma camp following an outbreak of fighting.
Our activities in Kenya in 2024
Data and information from the International Activity Report in 2024.
1.23
1.23
€24.4 M
24.4M
1987
1987
Featured
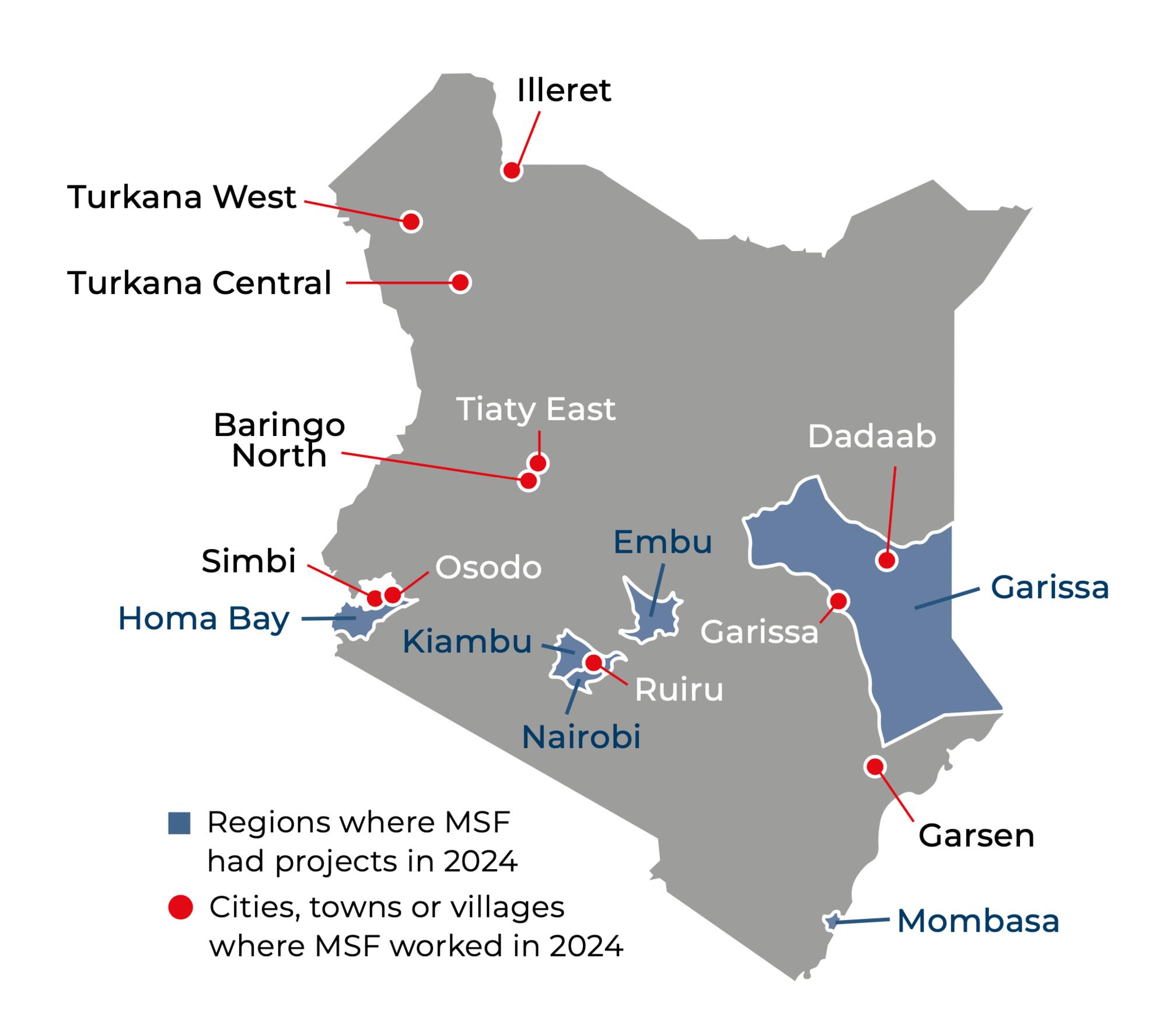
In Mombasa, we supported three health facilities to cater to the specific needs of vulnerable adolescents and young adults, such as people with disabilities, the LGBTQI+ community, individuals living on the streets, and people who engage in sex work or use drugs.
In Nairobi, our Lavender House clinic offered medical care and social support to people affected by violence – including sexual violence – in the Eastlands area. During the protests in July, our clinic dispatched a medical team to treat the injured. Our youth-friendly centre also continued to run medical services, psychosocial support, recreational activities, and educational programmes throughout 2024.
MSF responded to several other emergencies during the year. In March, extensive flooding resulted in hundreds of casualties, and destroyed homes and livelihoods. Our teams launched responses in Nairobi, Nakuru, Homa Bay, Tana River, and Garissa counties, providing medical assistance, as well as clean water, jerry cans, and warm clothes for children. We also responded to outbreaks of malaria in Baringo and Turkana counties, measles and Rift Valley fever in Marsabit county, and measles in Dagahaley camp. In the displacement camps in Baringo county, we launched a response to support victims and survivors of sexual and gender-based violence.
In Homa Bay county, we continued to run two adult wards, the tuberculosis ward, a Kaposi’s sarcoma clinic, and a post-discharge clinic at the hospital, as well as chronic disease clinics in two health centres.
After five years of supporting the provision of health and social support for people who use drugs in Kiambu, we handed over activities to the county Department of Health and a patient-led community-based organisation.
IN 2024

334,900
334,9
17,500
17,5
7,220
7,22
3,670
3,67


Breaking down stigmas and barriers to care in Mombasa, Kenya

Addressing sexual and gender-based violence faced by communities displaced by conflict in Baringo

Treating People Who Use Drugs in Kiambu, Kenya

Creating a safe space for the youth of Nairobi

