In the internally displaced camp near Malakal town in Central Upper Nile State, South Sudan, Dhan Tap looks sadly at a photo on his mobile phone. The picture isn’t much to look at –a tattered white rope hanging from the grass-thatched roof of a typical South Sudanese home.
“This rope was used by a 13-year old boy who hung himself,” he says. “Many of our patients –whether adults or teenagers - feel there is no future for them. [This] boy felt his parents could no longer support him while in the displacement camp and felt trapped, helpless.”
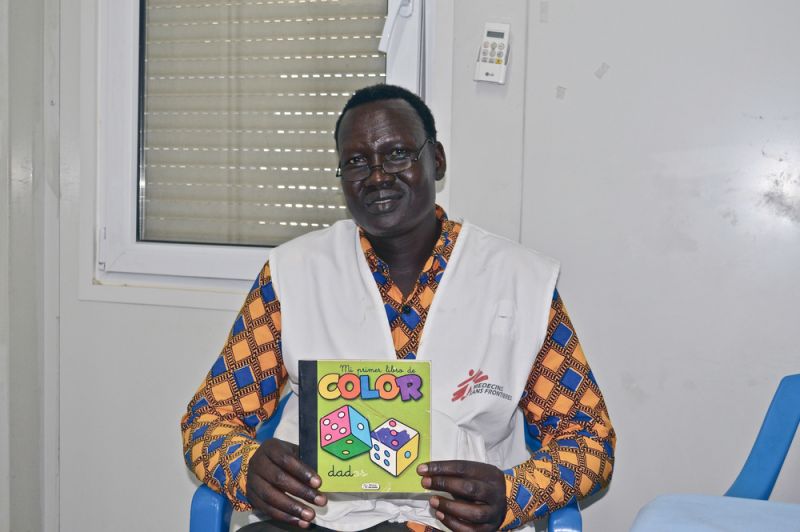
Dhan Tap, who himself fled from conflict in the area, works as a mental health counsellor in the internal displacement camp in Malakal for Doctors Without Borders (MSF).
Over the years, Tap has seen an increasing caseload of patients suffering from mental health conditions, often linked to their experiences of past displacement and future uncertainty.
From January to October 2018, MSF’s Malakal mental health team have supported roughly 30 new patients per month –one new case a day, of whom half struggle with serious mental health conditions including attempted suicide, says Tap’s colleague, Dr Jairam Ramakrishnan.
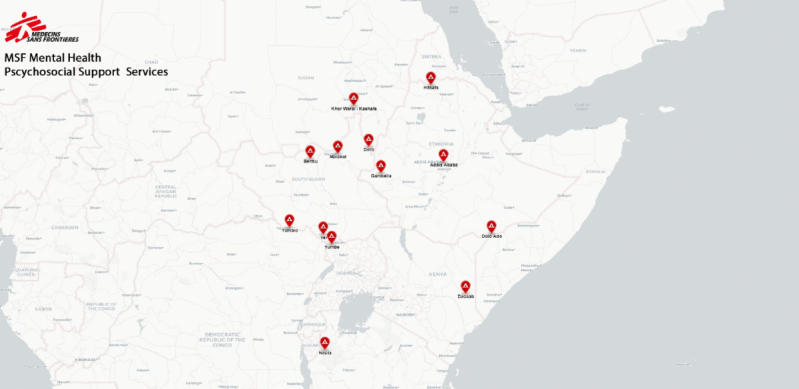
With the exception of Dadaab Refugee Camp in Kenya, where predominantly Somali refugees have been gradually repatriated since late 2014, nearly all MSF mental health programmes in the East and Horn region have seen a significant increase of patients. This includes projects in Ethiopia, South Sudan, Sudan, Tanzania and Uganda.
To meet mounting needs, MSF mental health projects, including individual counselling and group activities, have more than doubled in the past four years in Ethiopia, Sudan and South Sudan, according to MSF Mental Health Advisor María Cristóbal. In 2017, activities increased by 35% compared to 2016.
A spike in cases also occurred last year in Nduta Refugee Camp, Tanzania, for instance, that hosts over 100,000 Burundian refugees. According to Nduta’s Mental Health Activity Manager Monika Bregy, the camp saw the number of mental health cases per month double from 700 in July to more than 1,400 in August.
The number has since decreased this year in line with the diminishing refugee population due to an ongoing repatriation process.
More outreach, more acceptance
The increased caseload of mental health patients partly reflects the fact that the issue becomes more visible, with the increase of outreach activities and, consequently, of the awareness among the affected populations.
In Yumbe, northern Uganda, a town that hosts the largest refugee settlement in Africa, MSF Community Health Educators such as Emmanuel Rambo travel across the expansive camp to inform and encourage the camp’s residents to take advantage of MSF’s mental health support services.
Rambo is South Sudanese, twice displaced by conflict from his hometown in Yei, and relates easily to the predominantly South Sudanese refugee population in the camp. “There is a stigma within the community –people do not understand what mental health is, some associate it with witchcraft,” Rambo said. “And yet there is a huge need for mental health among this population, many have experienced physical assault, some have seen relatives killed.”
When displaced, distress follows
The lines of patients seeking mental health consultations in Yumbe are always long; MSF conducts on average around 900 consultations per month. “But I suspect we are only seeing a fraction of those who need our [mental health] support,” he added.
Rambo and his colleague Vastine Tayebwa, clinical psychologist, believe there is one main factor that triggers the high number of mental health patients MSF teams are contending with in Yumbe: displacement. “It’s the sense of loss, past traumatic experiences and future uncertainty that these refugees are facing,” Tayebwa says, gulping down a glass of water at MSF’s facility in Yumbe amidst the sweltering noon-day heat before hurrying back to provide further counselling.
“So far this morning I have seen six patients and already four more are waiting,” she says, gesturing at a growing queue of patients sitting patiently in silence outside her consultation room.

While a September 2018 peace agreement signed by the South Sudanese government and several rebel factions has relatively stabilised conditions, many refugees struggle with experiences from their past.
MSF’s affiliate medical research facility based in Paris, Epicentre, conducted a unique survey among nearly 10,000 refugees entering Yumbe camp in 2017 and found nearly all – 99.9 percent – of the refugees left South Sudan citing attacks on their village of origin or neighbouring villages.
A 2012 WHO report claims mild or moderate mental health disorders can rise up to 20 percent during emergency situations such as conflict-related displacement.
Dr Jairam Ramakrishnan and Dhan Tap share similar experiences to those in Yumbe, treating internally displaced South Sudanese patients from the formerly bustling city of Malakal. “Before the latest conflict set off in Malakal in 2013, people considered this town a safe-haven, but the war destroyed this image along with the sense of security for the people,” Tap said.
“That sense of loss and being uprooted from your life…it definitely takes its toll on you.” Dr Ramakirshnan considers the risk factors associated with people’s experiences in Malakal a “perfect storm” for developing mental health problems. “There is absolutely no doubt in my mind with the chronic conflict and lack of social support --this displacement makes a fervent ground for severe mental health patients.”

Displaced South Sudanese refugees who fled north into neighbouring Sudan reflect a comparable narrative to those who fled south into Uganda and those internally displaced within the country. According to Mental Health Supervisor Rania Abdel Kheir, it is the refugees’ exposure to traumatic events with less access to coping mechanisms and control over their lives that have incurred an increase in patients seeking counselling.
Rania Abdel Kheir works for MSF in the two refugee camps bordering South Sudan in White Nile State, Khor Waral and Kashafa Camps, and has witnessed since the project started in August 2017 an increase of 40 – 50 new cases per week. “The majority of them come from the conflict –some say they have lost relatives, some have even seen relatives killed in front of them.” While acknowledging the resilience of the people she treats in the camps, “even the strongest” she says, “would be affected by such kinds of experiences.”
Experiences of conflict and violence in the East and Horn regions make up 48 percent of the events (and risk factors) affecting people’s mental health, María Cristóbal says. The second leading causal factor based on gathered data is related to separation, making up 24 percent of the cases.
If indeed a correlation between displacement and mental health exists, the exceptional levels of displacement in the East and Horn region in 2018 would suggest an inevitable rise of mental health problems among the uprooted populations.
The UN reported an unprecedented number of people were displaced in 2017, with nearly 70 million people either internally or externally displaced. Out of these, roughly a fifth emanated from the East and Horn region, according to the 2018 Global Report on Internal Displacement.
In countries like Ethiopia, host to the second largest refugee population in Africa, these numbers are set to continue. The UN warns that, despite a peace agreement between Ethiopia and Eritrea, conditions within Eritrea remain unchanged while the border between the formerly restive countries has opened up. This new porous border allows a fourfold increase in Eritrean refugees entering Ethiopia, with most going to Hitsats Refugee Camp in the northern Tigray region of the country.
Displacement can trigger mental health conditions at varying stages –whether in transit or while eking out an existence within a camp. The leading symptoms cited by MSF in the East and Horn region include: anxiety, depression and psycho-somatic conditions, Cristóbal says.
Although there are no concrete ways to directly measure mental health problems caused by personal experience, certain trends are apparent. In the cases of Yumbe in Uganda and Hitsats in Ethiopia, experiences of PTSD and severe depression appear most common. “I counselled one rape survivor, 20 years old, whose family members were killed by armed men,” Tayebwa said.
“To make matters worse, the woman had been forced to eat the meat of a dead person –a relative, before she was set free,” the patient told Tayebwa.
“These terrible memories can remain with someone for a long time.” In Hitsats, many of the exiled Eritreans had faced imprisonment, mistreatment and life-threatening situations crossing the border to Ethiopia. According to the Mental Health Supervisor at Hitsats, many are struggling with traumatic experiences such as PTSD but also severe depression as they grapple with an uncertain future.

Depression and psycho-somatic conditions constitute the main symptoms identified in Malakal. “Given the violence that people have lived through, many would be expected to suffer from post-traumatic disorder. But I see a different picture,” Dr Ramakrishnan said. “
Despite the violence, people are resilient and survive without many of the tell-tale signs of post-traumatic stress disorder. But over time, faced with being stuck in the current living circumstances without any improvement in their lives, [they] feel hopeless.” On average, there are around four suicide attempts in the camp per month, according to Psychologist Diana Sochitl Rodríguez.
No health without mental health
If these and other mental health disorders are ignored, there is a risk these symptoms can mutate into physical illnesses and potentially contribute to further societal challenges. Mental disorders increase the risk for contracting communicable and non-communicable diseases, according to a 2007 Lancet report, and are linked to as much as a third of all non-communicable illnesses.
“Mental and physical health is like one coin –when there is disease in your mind, it affects you physically –it’s one coin,” Tap said. “When the mind is affected it will lead to the body.” Even the lifespan of people with severe mental health conditions is shorter compared to the general population, according to Cristóbal. A 2005 World Health Organisation (WHO) estimate shows mental disorders accounting for 1.2 million deaths every year.

Untreated and undiagnosed mental conditions are also affecting society in South Sudan, says Dr Garang Apiu, a general practitioner in Juba. “I have made it a mission in life to treat those who need help and those who don’t even know they need help –otherwise the remnants of this war will haunt us mentally for the rest of our lives if left unchanged,” Dr Apiu said.
Cases of alcoholism, a tendency towards aggressive behaviour, including domestic violence, in South Sudan may be linked to mental conditions, he believes. “PTSD and depression are hardly diagnosed due to the fact that alcoholism is not seen as an illness and neither is the tendency to violence seen as a serious manifestation of mental disorder. Mental health-linked violence has become normalised,” Dr Apiu added.
Yet despite the serious implications of leaving mental disorders untreated in the East and Horn of Africa, mental health services in the region are either woefully inadequate or non-existent. WHO estimates 540 million people worldwide suffer from mental health disorders, nearly 75 percent of them living in low and middle-income countries.
Resources to prevent, identify and treat mental health problems are particularly scarce in the African region, WHO reports, with less than 20 percent of people having access to mental health care and just one psychiatrist for one million people.
War-torn South Sudan has less than a handful of trained psychiatrists working within the country, Dr Apiu said. “With the current staff we are just drops in the ocean,” he added, “within the medical community in South Sudan, few believe in the importance of this field.”

Since last year in South Sudan, MSF has worked with a group of government and non-government organisations to help reintegrate child soldiers in the southwestern town of Yambio back into their communities.
Some communities fear accepting former child combatants into their homes and some children carry the burden of guilt about their experiences or, sometimes, about being captured and taken from their homes, says Carol Mwakio Wawud, a psychologist with the programme. Such cases require more than individual counselling or medical attention: it takes a whole community to ensure future mental welfare.
Quite often the few mental health support services available inevitably become stretched further than planned. In Khor Waral and Kashafa Camps, Sudan, MSF services have ended up supporting six camps and the host community. “We are definitely stretched,” said Rania Abdel Kheir.
“Even if mental health support is available, often it is not the right type of support,” the Mental Health Supervisor continues, “with only one psychiatrist; for instance, you cannot provide important, specialised services.”

Despite these challenges, mental health support remains relatively cost-effective, according to a 2015 paper by the U.S.-based Center for Global Development. “When providing mental health and psycho-social support, we don’t need medical samples or demanding technical devices,” says Nduta’s Mental Health Activity Manager Monika Bregy.
“Compared to the medical care provided in Nduta project, the costs for mental health support are minor.” Tap agrees. “It’s often more about time and patience than financial costs.”
Tap uses simple tools such as games, children’s books and toys to help children struggling with mental health issues in Malakal, South Sudan. “When you see children playing again, you can see that not all is lost.”
Read more about Mental Health in Africa here.
