AIDS IS NOT OVER: Address inequalities, accelerate inclusion and innovation
During the upcoming ICASA conference in Zimbabwe, MSF will share its experiences in working towards reaching people with adequate tools & strategies for both prevention and treatment. MSF calls on all actors to prevent the worsening of shortfalls undermining/weakening the HIV response and to redouble efforts to mitigate the neglect of the most vulnerable.

Triple neglect: vulnerable groups remain underserved and neglected by global efforts to fight HIV/ AIDS and Tuberculosis
In view of the upcoming World AIDS Day, MSF expresses its (deep) concern about the current uncertainty that hangs over the continued commitment to respond to the HIV pandemic.
30 million people rely on daily ARV pills to stay alive, pills that are largely only available as long as the world agrees to fund Global Fund and PEPFAR.
AIDS is not over, and we cannot afford to lose track or be distracted from mobilizing around the most effective response to save lives.
The consequences for patients and programs of gaps that MSF currently observes, illustrate the risks of significant losses of achievements or even rebound.
People with specific vulnerabilities that already now face neglect will be most affected. In particular, we want to raise the neglected needs of people in humanitarian crisis, of excluded population groups who are criminalized, marginalized, and discriminated against, and of patients in advanced stages of HIV disease without adequate detection, therapeutics and care.
Neglected crisis contexts
Uninterrupted provision of HIV & TB care in complex humanitarian emergencies remains one of the major gaps in the HIV& TB response. Humanitarian emergencies and armed conflicts, especially those with prolonged character, increase vulnerability and inequity among the affected populations, including the risk of HIV transmission and access barriers to HIV & TB care services. Updated data on gaps in HIV care in such contexts remain scarce, however in 2016, it was reported that out of 2.6 mil PLHIV affected by a humanitarian emergency, 1.43 mil could not access lifesaving treatment (54% of adults; 65% of children, 79% of adolescents and 43% of pregnant women). [fn]UNHCR and WFP 2019, Information note: HIV in humanitarian contexts[/fn]
MSF is witnessing disruption of HIV & TB services for the people in conflict areas such as Northern Mozambique, South Sudan, CAR or Eastern DRC. As an example, Cabo Delgado Province has a prevalence of HIV (13% among adults). The HIV program suffered disruptions for more than five years, which affected the equilibrium of services. When MSF started its support to the Hospital of Mueda district, 42% of the women who delivered in February 2022 were HIV positive, with only one on ARV, 55% of the children in the pediatric wards were HIV positive and 80% of the children in ITFC had HIV or TB. In Palma district, out of 5533 people ever enrolled in care, only 153 are still active in care today.
People living in these complex crisis contexts face significant challenges in accessing care. Insecurity, long distances to reach the facilities, and out-of-pocket expenses are among the main barriers.MSF

Other emergency situations, such as extreme/adverse weather events or epidemic outbreaks, cause similar problems. High numbers of patients with Advanced HIV disease, bad loss-to-follow-up rates, and high rates of mother-to-child transmission are noted as consequences of an unadapted supply chain, lack of decentralization of services or insufficient patient autonomy. Issues concerning the availability and access of testing, AHD screening, prevention & treatment at the PHC level, and trained health workers hamper services, both in quantity & quality, further complicated by stigma & discrimination. A lack of respondents that include key HIV & TB services systematically during crises and the inexistence of contingency plans need to be addressed.
The current war in Ukraine showed the complexity of adapting the response to answer the needs of patients with chronic diseases but also provided positive lessons learned on the capacity of actors (international such as UN agencies and local CSO) to mobilize to ensure continuity of care to people in need. The CSOs have been the backbone of the response in Ukraine, with consistent support by humanitarian and international health actors.
The COVID-19 pandemic showed the world that no place/no country is exempted from the need to plan for the unexpected. Considering the perspectives of crises linked to climate change, conflict, epidemic outbreaks and the risk of pandemics, preparedness of HIV & TB services should get more priority, reflecting the ‘new normal’ of emergencies or humanitarian settings to be expected.
People living in those complex crisis contexts face major challenges in accessing care. Insecurity, long distances to reach the facilities, and out-of-pocket expenses are among the main barriers.

Neglected people: “the deliberately excluded”
Additionally, some people face important barriers to prevention & care linked to social, cultural and legal restrictions.
Stigmatization, discrimination, conservative laws regarding the age of access, criminalization of sex work, drug use or same-sex sexual relations are harmful to the people and communities; they undermine efforts to fight against HIV/ AIDS. Key populations are paying the brunt of these policies and practices.
Suppressing harmful laws and policies, implementing legal instruments to protect the rights of the people and implementing strategies with peers are the ways forward to improve access for neglected people.

Neglect to ensure key tools
Implementing new tools is also a big challenge today, in all contexts. The basic package for screening, prevention and treatment of advanced HIV disease is not yet systematically implemented in all countries, despite clear WHO guidelines existing for several years and a growing attention from donors to this intervention.
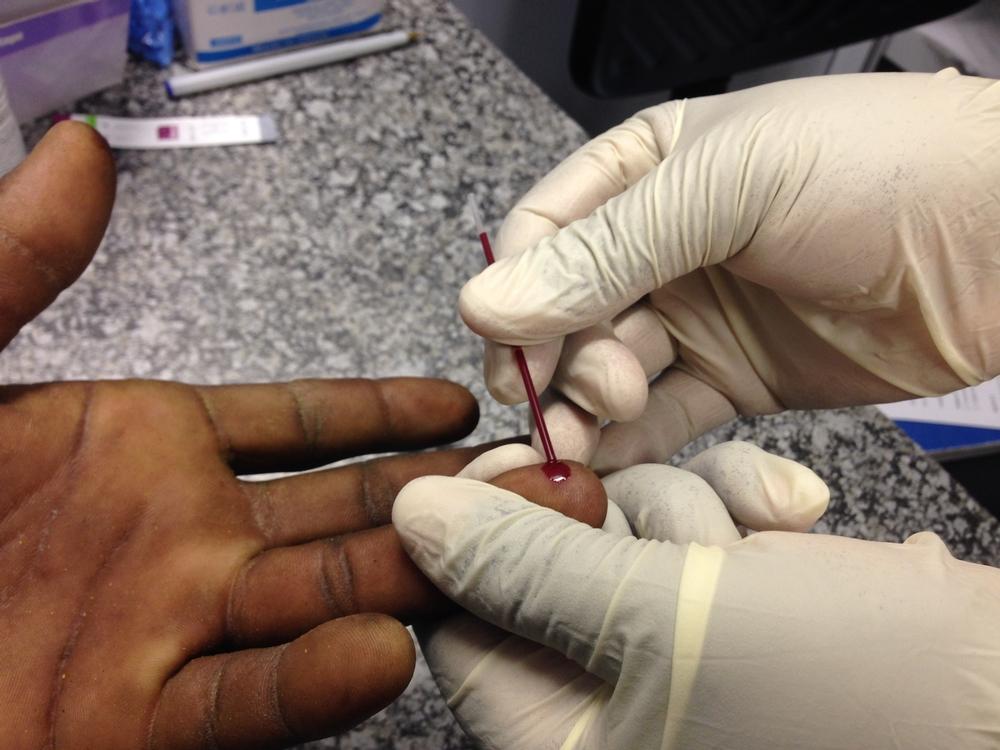
The basics, such as access to CD4 testing, are under threat with the decline of interest from key manufacturers of CD4 point of care (POC) machines, despite its key role in the diagnosis of advanced HIV cases among PLHIV.
While the inclusion of less toxic treatments for cryptococcal meningitis, recognition of severe bacterial infections and a focus on Kaposi’s Sarcoma in the AHD package is becoming a clear way forward for a better impact on morbidity and mortality of people living with HIV, concrete political commitment and translation into concrete action are still lacking.
The long-acting, most effective tool for the prevention of HIV - Cabotegravir long-acting ( CAB-LA) is another example of a new tool that has not been prioritized for use in the most vulnerable populations. With only a single manufacturer with limited supply capacity for the near future, ensuring equitable distribution of this drug to those settings and populations most at risk is essential to reach the 2030 targets for new HIV infections.
Political commitment and translation into concrete action plans as the way forward
To overcome this triple neglect, political commitment from all actors is needed to have the necessary support and funding to act. In this matter, the current uncertainty brought by the non-reauthorization of PEPFAR is not a positive sign for pursuing ambitious actions that accelerate and innovate the response.
MSF will organize and participate to several events and sessions to bring those topics during the ICASA conference.

Microplanning HIV and SRH services to key populations in Mozambique.

https://youtu.be/jLXE2ynR7H8
| Date | Time | Satellite Name | Venue | MSF Speaker |
| 6 December 2023 | 17h30 | Side-event Missing in action: HIV & TB during emergencies and humanitarian crisis | Monomotapa Hotel | Stephanie Dreze HIV Advocacy Coordinator |
| 6 December 2023 | 15h30 - 16h15 | Peer Educators as Harm Reduction Treatment Buddies | KP networking zone | Lelia Wairuimu: Kiambu KP Peer Edwin Kangethe: Kiambu KP Peer |
| 7 December 2023 | 13h05 - 13h50 | Lessons learnt in responding to HIV & TB service disruptions among conflict & natural disaster-affected populations | VIP Lounge | Tom Ellman: Southern Africa Medical Unit Director |
| 7 December | 13h05 - 13h50 | Diagnosis and management of advanced HIV disease | Jacaranda 123 | Amanda Banda: Access Campaign consultant or Antonio Flores: Senior HIV/TB Advisor |
Resources (reports, briefing papers, abstracts, posters)
Contact Us

Harare, Zimbabwe | Rainbow Towers, Harare



