
Community Health Agent Programme Toolkit
Introduction and Background
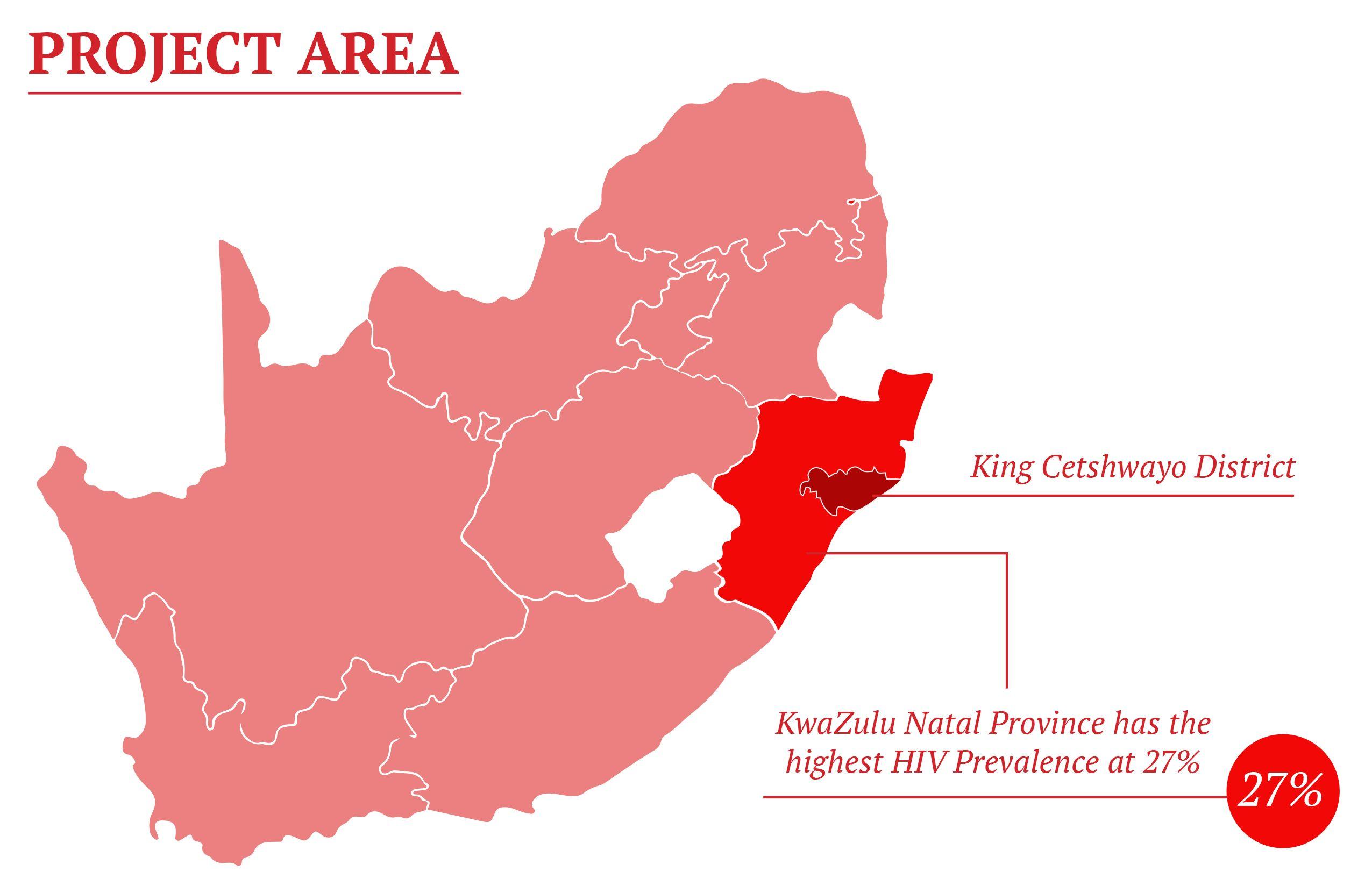
This ‘toolkit aims to guide the development of innovative door-to-door HIV Counseling and Testing (HCT) initiatives in settings where HIV prevalence is high, but where few can access testing services. The guidance is drawn from the experience of Médecins Sans Frontières/Doctors Without Borders (MSF) in establishing and running an effective, large-scale door-to-door HCT programme in parts of KwaZulu-Natal’s (KZN) King Cetshwayo District (formerly uThungulu District), in partnership with the KZN Department of Health.

Eshowe HIV project reaches 90-94-95
Challenges of HCT coverage in high HIV prevalence settings
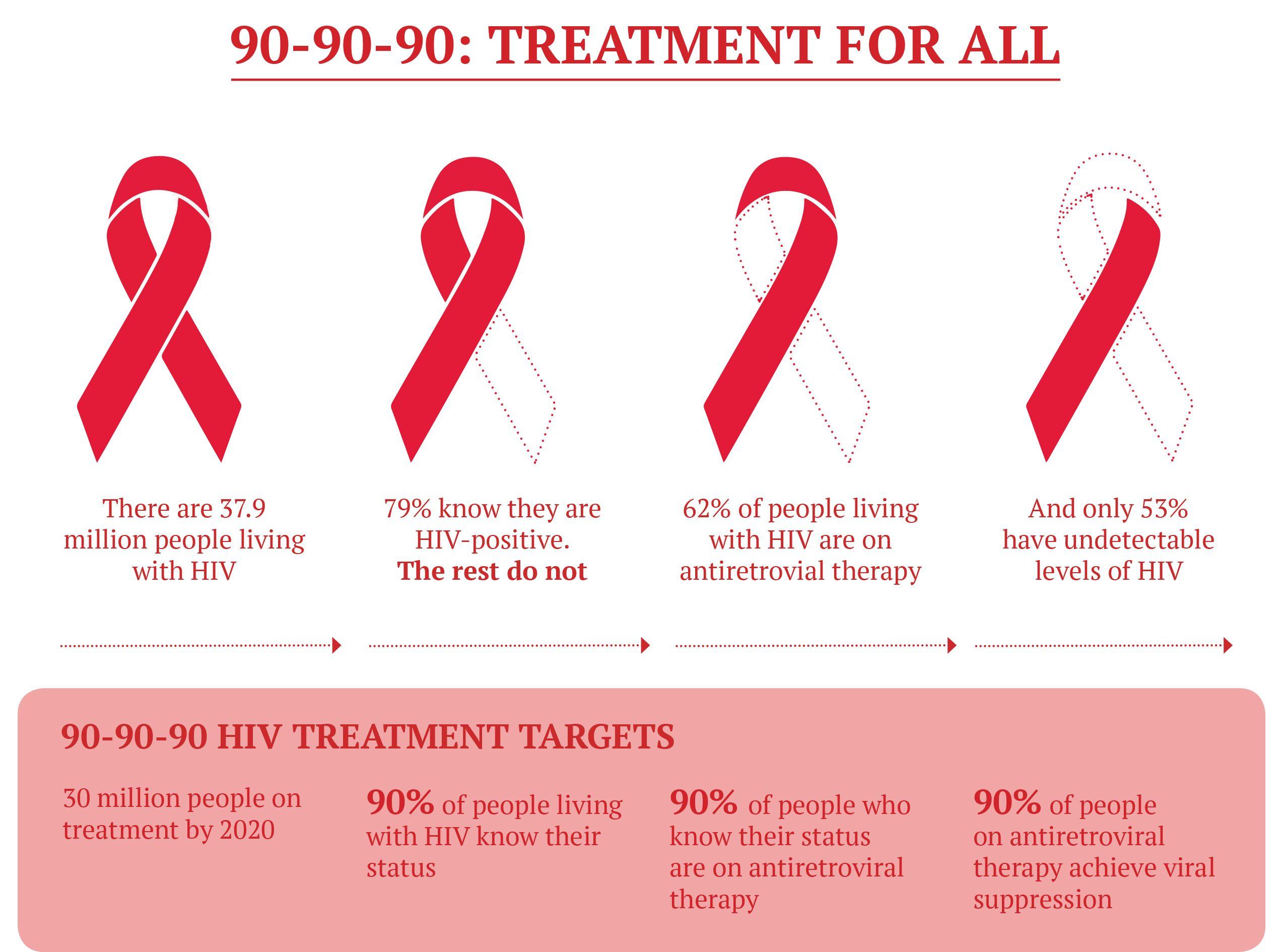
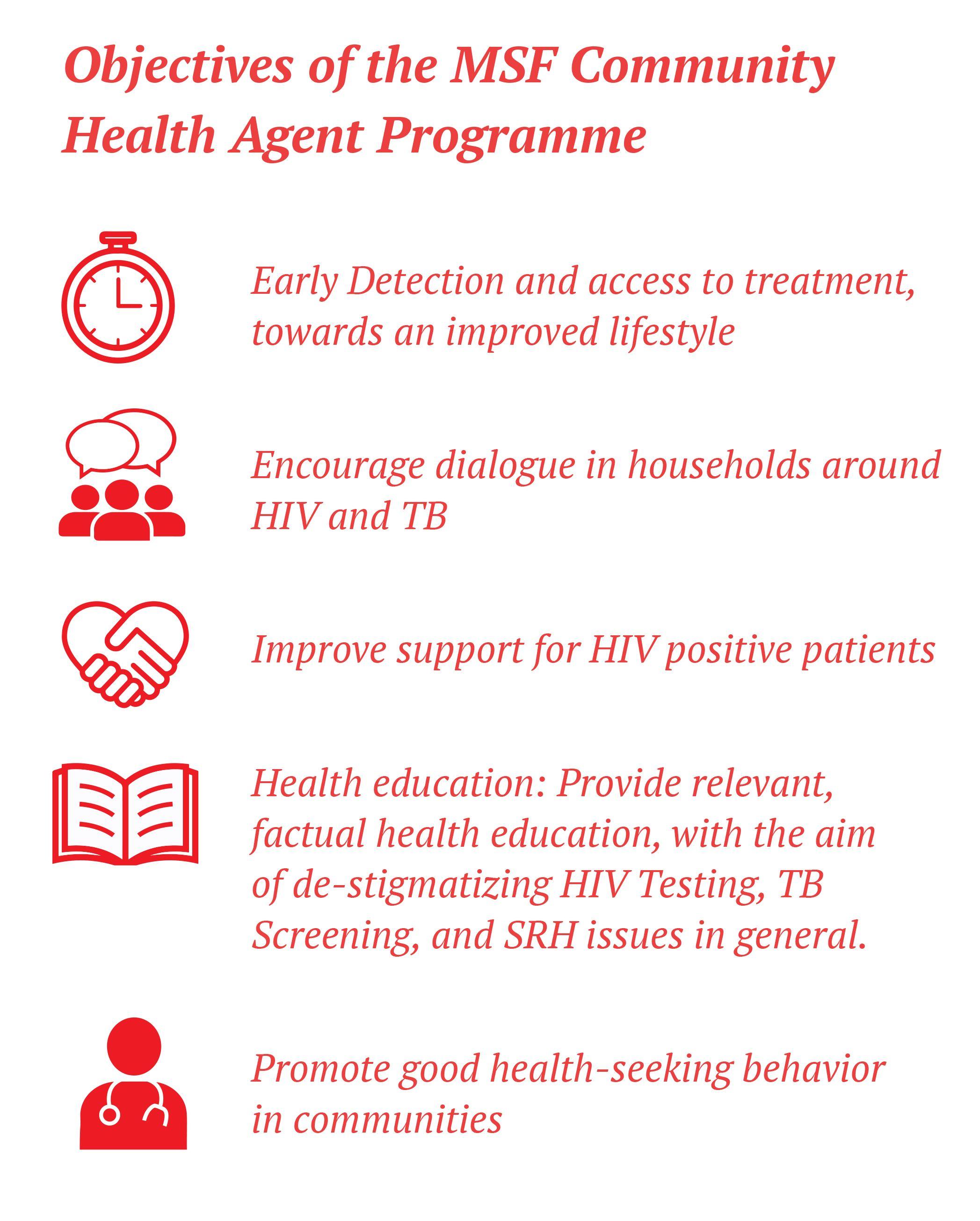
In April 2011, MSF in partnership with the KZN DOH started an HIV/TB project called ‘Bending the Curves’ in King Cetshwayo District (pop. 128 000), specifically targeting the town of Eshowe and rural Mbongolwane. The results of two major surveys conducted by MSF confirmed a very high prevalence of HIV in this area, and the MSF project was established with the aim of reducing the incidence of HIV/TB and bringing down HIV/TB morbidity and mortality – in other words, to bend the curves of the epidemic downwards, in line with the targets of South Africa’s National Strategic Plan on HIV, STIs & TB (2012-2016). MSF additionally sought to help the KZN DOH bring HIV under control, by achieving the UNAIDS 90-90-90 by 2020 targets in this area (see infographic below).
The hilly topography that characterizes this part of Zululand makes access to health services a challenge for many, contributing to a situation where almost 20% of adults between the ages of 15-59 were untested, and 25% of HIV positive individuals were unaware of their status. People who are not aware of their HIV positive status play a significant role in ongoing transmission of HIV, and the MSF project quickly developed a strategy for taking HIV education and testing services into communities.

However, due to lack of awareness in some rural communities, as well as spatial and financial barriers, HCT remains difficult to access for many people. Community-based approaches can broaden access to previously hard to reach populations, by bringing services closer to the people.

Community Health Agents Programme - CHAPS
Achieving 90-90-90 in Eshowe and Mbongolwane with door-to-door testing and other strategies
In 2018, MSF carried out an HIV Prevalence Survey in the Eshowe and Mbongolwane area, and the results showed that the project has achieved the UNAIDS targets of 90-90-90 two years ahead of the 2020 deadline, with results of 90-94-95. In other words, 90% of people living with HIV now know their status, 94% of those who know their status are on antiretroviral treatment and 95% of those on treatment have a suppressed viral load, meaning the virus is undetectable in their blood. Interventions at the community level are believed to have played a major part in this success. In the words of project medical referent, Dr. Liesbet Ohler, ‘Health workers providing door-to-door testing as well as linkage to care contributed significantly to the achievement by boosting HIV literacy and the uptake of testing in often remote areas where a high HIV prevalence went together with a low uptake of HIV services.’
PopART: use of community health workers in achieving population-level reductions in HIV incidence
The experience of MSF in King Cetshwayo District follows a wider trend of findings, most notable of which has been a recently published study examining the effect of universal testing and treatment on HIV incidence in areas of Zambia and South Africa, known as the PopART trial. The community randomized trial compared the effects of universal test-and-treat, which involves testing everyone at risk for HIV infection and immediately treating those who test positive, to the impact of treatment using local guidelines or standard of care.
A prevention intervention included home-based HIV testing delivered by community health workers (CHW), who also supported linkage to HIV care and ART adherence, similar to the package of care offered by the Community Health Agents in King Cetshwayo District. At each visit, CHWs offered HIV counselling and rapid testing, and they provided support for linkage to care and ART adherence for HIV positive clients. The study showed that the prevention intervention and ART provision according to local guidelines resulted in a 30% lower incidence of HIV infection than a standard of care. It also showed that universal testing and treatment reduced the population-level incidence of HIV infection (Hayes et al., 2019).
Read more here

Community Health Agents Programme
The programme was developed in conjunction with local leadership and implemented in partnership with the Shintsha Health Initiative (SHINE), a local HIV NGO founded by a group of women living with HIV.
The door-to-door testing program developed by MSF was named the Community Health Agents Programme, henceforth referred to as The Programme for short. Launched in October 2012, The Programme was one of several HCT strategies deployed by MSF in Eshowe and Mbongolwane aimed at dramatically raising the coverage of HCT in communities and driving improved linkage to care. The comprehensive HCT strategy of the MSF project additionally comprised fixed testing sites in urban and rural areas, HCT support to health facilities, and mobile services.
The programme was developed in conjunction with local leadership and implemented in partnership with the Shintsha Health Initiative (SHINE), a local HIV NGO founded by a group of women living with HIV. Child Care South Africa took over from SHINE in March 2016, and in 2018 the programme was closed. According to Ntombi Gcwensa, MSF Patient Support Manager in Eshowe, ‘analysis of our 2016/2017 results indicated that the yield of HIV positive individuals in the programme had decreased a lot and that our agents were testing mainly the older generations and the very young.
A decision was taken by MSF and the local DoH to close the programme, and to focus on establishing community health posts in key rural hubs.’ Several of the community health agents have found employment in these health posts, which offer HCT; Condom Education & Distribution, screenings for TB & STIs, pregnancy testing, screening for diabetes and high blood pressure; contact tracing and defaulter tracing; health education; and more.

Developing a Door-to-Door testing programme
Effective door-to-door services to help fight HIV
Step 1: Research, Design & Consultation
1.1: Assess the healthcare gaps
Door-to-door services can be a very effective weapon in the fight against HIV, particularly in contexts where people struggle to access health facilities, and/or where facilities lack the resources to provide HIV services like HCT.
To assess the need for door-to-door services in an area, the following steps are recommended:
- Obtain existing HIV statistics for the focus area
- Assess HIV testing practices at local health facilities
- Assess access to health facilities
- Assess the coverage and capacitation of community-based HIV testing sites, including sites supported by non-governmental actors

The findings of that survey helped MSF and the DoH to implement activities and adapt strategies in the sub-districts, among them the Community Health Agents Programme. A similar survey was implemented five years after the first one, as part of an evaluation of the changes in the HIV epidemic and the cascade of care since 2013.
**See KZN Mbongolwane & Eshowe HIV Impact in Population survey under reference.
1.2: Mapping
- Obtain copies of up to date area maps, including topographic maps, road maps and most important of all: an administrative map of the area, clearly demarcating all administrative areas
- Source information on relevant administrative dynamics at all levels of governance
- Obtain demographic information for each administrative area
- Establish population size
- Establish gender and age ratios
- Establish the number of households
MSF experience: Mapping
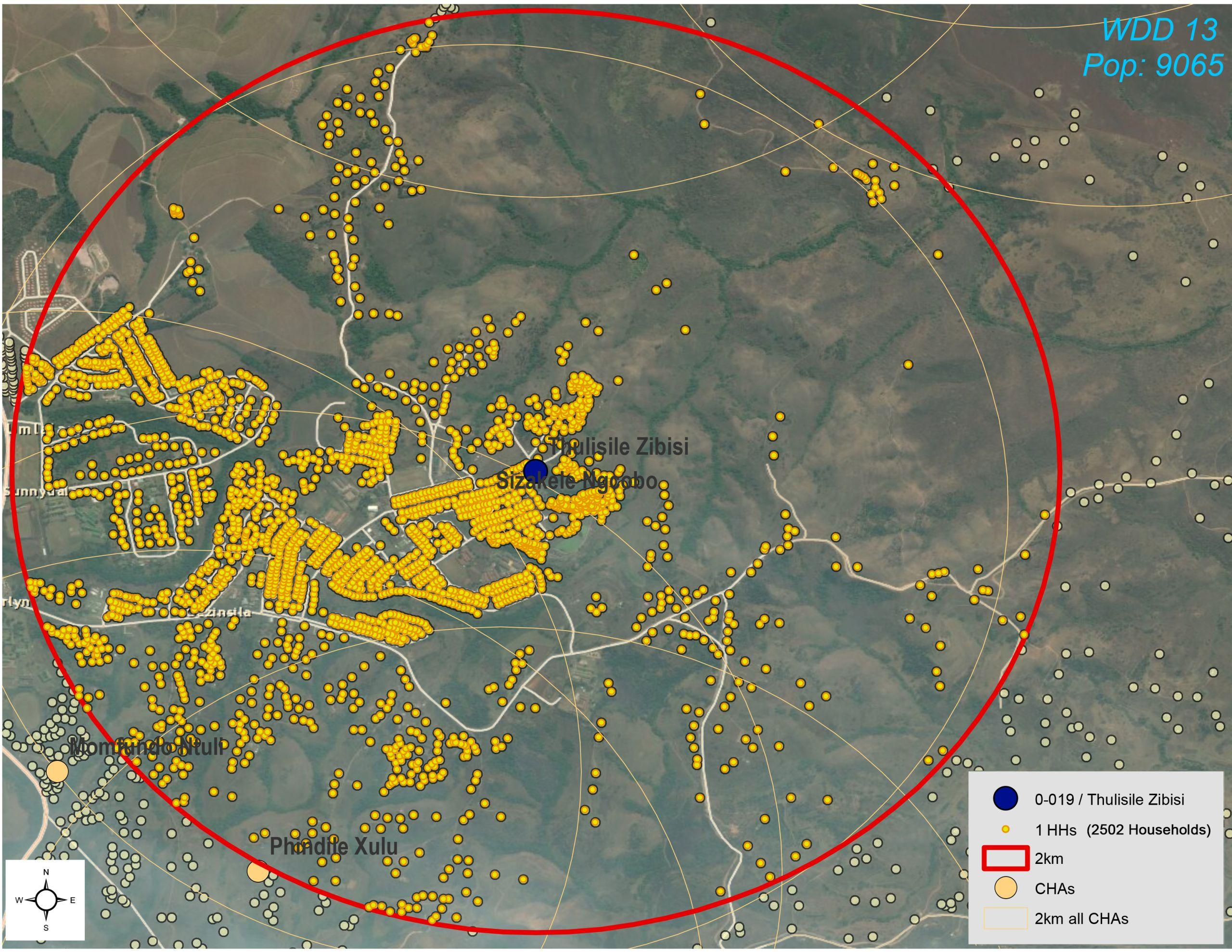
i. According to MSF logistician Khayo Nzuza, administrative maps for the project area were obtained from the municipality office, whereas population data was drawn from the Statistics South Africa national census 2011. ‘The municipal office was our source for information on municipal ward boundaries as well as the boundaries of traditional wards, known as isigodi. In this part of KwaZulu-Natal governance is multi-layered, and it was important to form an understanding of all the different systems of leadership that are present. The easiest way to start doing this was to map them.’
ii. Municipal boundaries and traditional boundaries in the project area were not the same, and ensuring an understanding of both was essential to the management of the programme.
iii. Once the programme was up and running, the location of each community health agent was plotted on a map of Umlalazi Location using a programme called ArcMap, supplied by ESRU South Africa

1.3: Consultation
Meaningful consultation with local authorities, traditional leaders and local community-based organizations is essential when designing community HCT intervention, as social dynamics differ and what works in one area might not be an appropriate approach in another. In the area of KwaZulu-Natal in which MSF operates traditional leaders are very influential, and securing the support of these leaders proved an essential step. There is no single recipe for securing the buy-in of relevant authorities, but the following actions should be taken at the minimum:
- Consult carefully with established NGOs and community-based organizations
- Engage relevant government and traditional/community authorities, making the case for the proposed intervention respectfully and compellingly
- Discuss the recruitment procedure with administrative and traditional authorities
- Meet with essential role-players as often as is necessary to achieve full mutual understanding and support

MSF experience
In Eshowe and Mbongolwane, MSF consulted important stakeholders from the outset. These included:
- The Department of Health at the Provincial, District and sub-district level
- Hospitals and Clinics in the project area
- Traditional leaders (Amakhosi, Izinduna)
- Municipal Ward Councillors
- Religious leaders
- Other Non-Government Organizations/Community-based organizations
- Community Health Workers employed by the DoH
- Traditional Health Practitioners (Izinyanga, Izangoma)
Engaging traditional leaders was a particularly important step in the development of the programme. MSF started by identifying all traditional leaders within the target area. Staff visited traditional leaders one by one with the aim of introducing the organization and explaining the programme objectives. ‘We immediately realized we faced a challenge, because many of the traditional leaders lacked HIV literacy themselves, and therefore how could we expect them to carry our messages to their communities?’ Ntombi recalls.
To address this issue MSF offered HIV trainings in several areas to the traditional council made up of 30 community representatives. ‘We then visited the Indunas in each ward and explained the programme, making it clear that we required their help in organizing community gatherings, and with identifying the right individuals within the community to work for MSF as community health agents, delivering the programme’s envisaged services.’

1.4: Select a partner for community-based implementation
To identify the right partner, the following steps can be undertaken:
- Conduct research aimed at ‘mapping’ local organizations
- Put the work out to tender, placing advertisements with local media outlets (newspapers, radio stations)
- Invite individual organizations to pitch for the work
MSF experience: working with passionate activists
While it is preferable to partner up with a local organization to deliver community-based services, it could be the case that no relevant local organization exists. When MSF was developing the programme in King Cetshwayo District in 2012 there were no local HIV organizations, and so MSF supported a group of women living with HIV to form the Shintsha Health Initiative (SHINE).
SHINE became a major force in the fight against HIV in the area. Supporting the formation of a local HIV organization is one potential answer if no suitable local organization exists, however it is important to note that this strategy comes with its own challenges, such as ensuring the organization follows sound management practices.

1.5: Finalize details of the programme
Taking all research findings and the input of local authorities and organizations into account, providers must resolve the following questions:
- Where to work and the number of staff required
- What service package will be provided
- What the programme objectives and targets will be (for example, who to target; number of HIV tests to be performed per year; the number of times each household is visited, etc.)
MSF experience: Determining a package of services
When MSF launched the programme in 2012 two main activities were offered: HIV counselling and testing (HCT) and TB screening, with linkage to care as required. In time the programme service offering was expanded to include the following services:
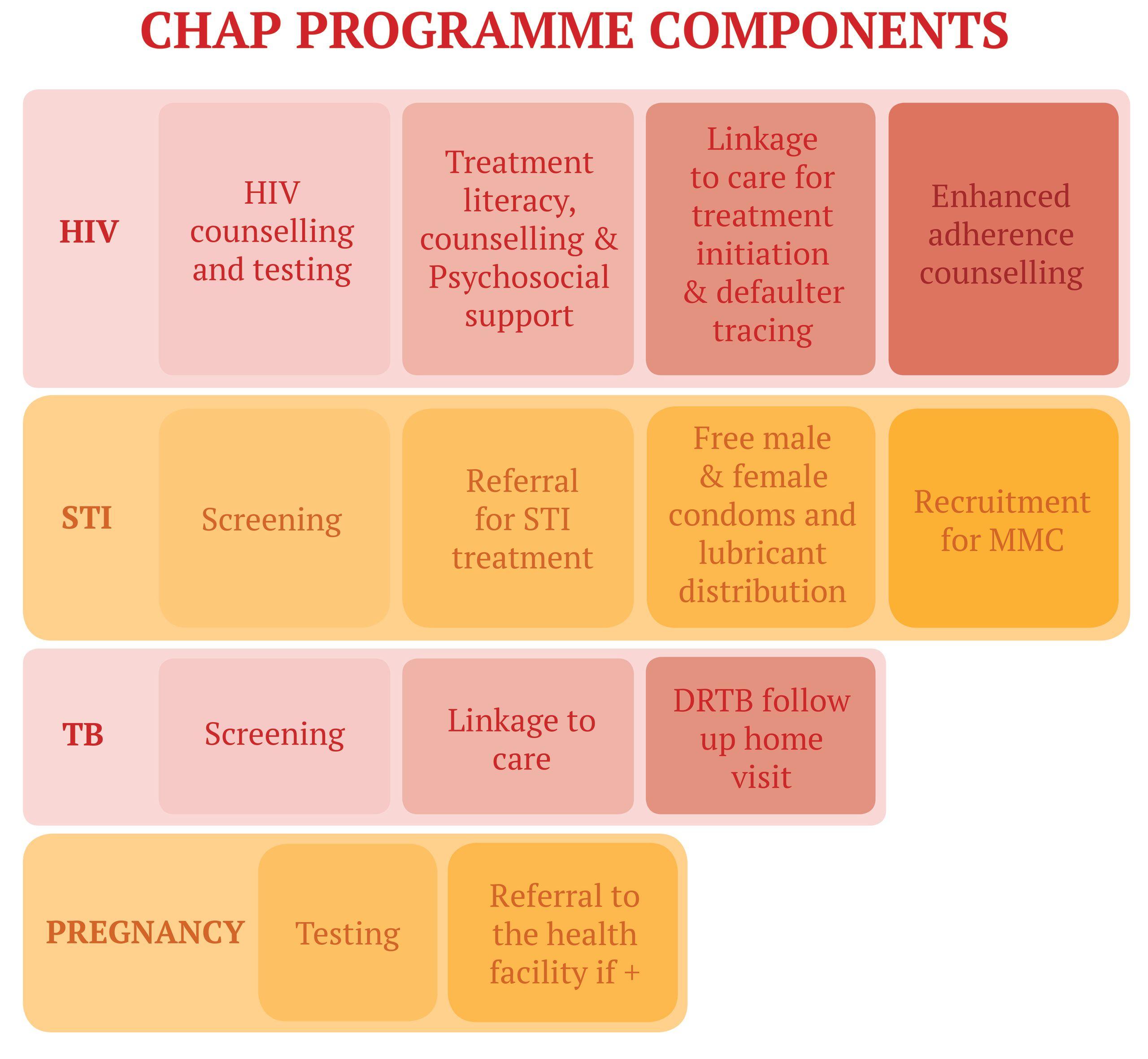
MSF experience: Setting targets
The programme initially prioritized issues of coverage (getting to as many households within the project area as possible) over the achievement of specific targets. In 2012/13 individual community health agents conducted 8-9 HIV tests a week on average. By 2017 the weekly target for individual community health agents had risen to 16 tests.

Organize the programme with health authorities and partnering facilities
The following actions can help to ensure smooth collaboration with local authorities and partners:
- Establish a reporting system, deciding what format reporting should take, how frequently reports should be filed, what data is to be collected, and how and to whom it should be reported
- Explore whether consumables (i.e. HIV and pregnancy test kits, gloves, cotton wool, etc) can be provided by DoH, understanding that it may take the DoH some time to work these expenses into their budget, and these expenses might fall to the provider in the interim
- Provide DoH with detailed projections of what resources will be required
- Ensure partnering facilities dispose of medical waste responsibly in line with prescribed national standards.
MSF experience: sharing the workload
It is highly recommended that the local authority take responsibility for all consumables and the disposal of medical waste from the outset. A 2017 costing study of the programme revealed that consumables are the lowest cost item, accounting for 0.11% of total expenditure. However, having the local authority take responsibility for the cost of consumables from the outset helps to ensure a committed partnership and sustainability of the door-to-door testing initiative to the local health authority.
1.7: Validation of program by local authorities
Present the final plan to local authorities and secure approval.
MSF experience:
Community Health Agents Programme was incorporated into the Memorandum of Agreement signed by the MSF project coordinator and the KwaZulu-Natal Department of Health. A co-signed Memorandum of Agreement, or Memorandum of Understanding, is the ideal form of approval. Respectfulness and humility were key – being pushy and forcing the pace of operational roll-out only led to setbacks.
Step 2: Recruitment & Training
Having determined where to work and what services will be offered, the human resources structure of the programme can now be developed, followed by recruitment of staff and – ideally at the same time - the development of required training modules.
2.1: Finalize HR Structure
The number of community health agents required to drive a door-to-door testing programme will be determined by
- The size and density of the population to be reached
- The size of the catchment area
- Monthly programme targets (how many households must be visited per month, how many tests to be performed, etc)
- Estimated daily workload
For guidance on how many community health agents are required to drive a successful community-based HCT programme refer to the South Africa National Department of Health 2019 - 2024 Policy Framework and Strategy for Ward-based Primary Healthcare Outreach Teams [Reference] more commonly called WBOT(‘s). The policy says that 9159 WBOTs and 54956 Community Health Workers (CHW) are needed to serve the entire South African population, and that WBOTs will be responsible for approximately 6 000 individuals or 1 500 households. However, the policy advises that the actual number of households covered by each team of CHWs will be influenced by:
- distance and travel time between households
- demographic characteristics of the population
- burden of disease
The policy also advises that the ratio of WBOTs to both individuals and households ‘may be changed in the future based on evidence from research that is being conducted’.
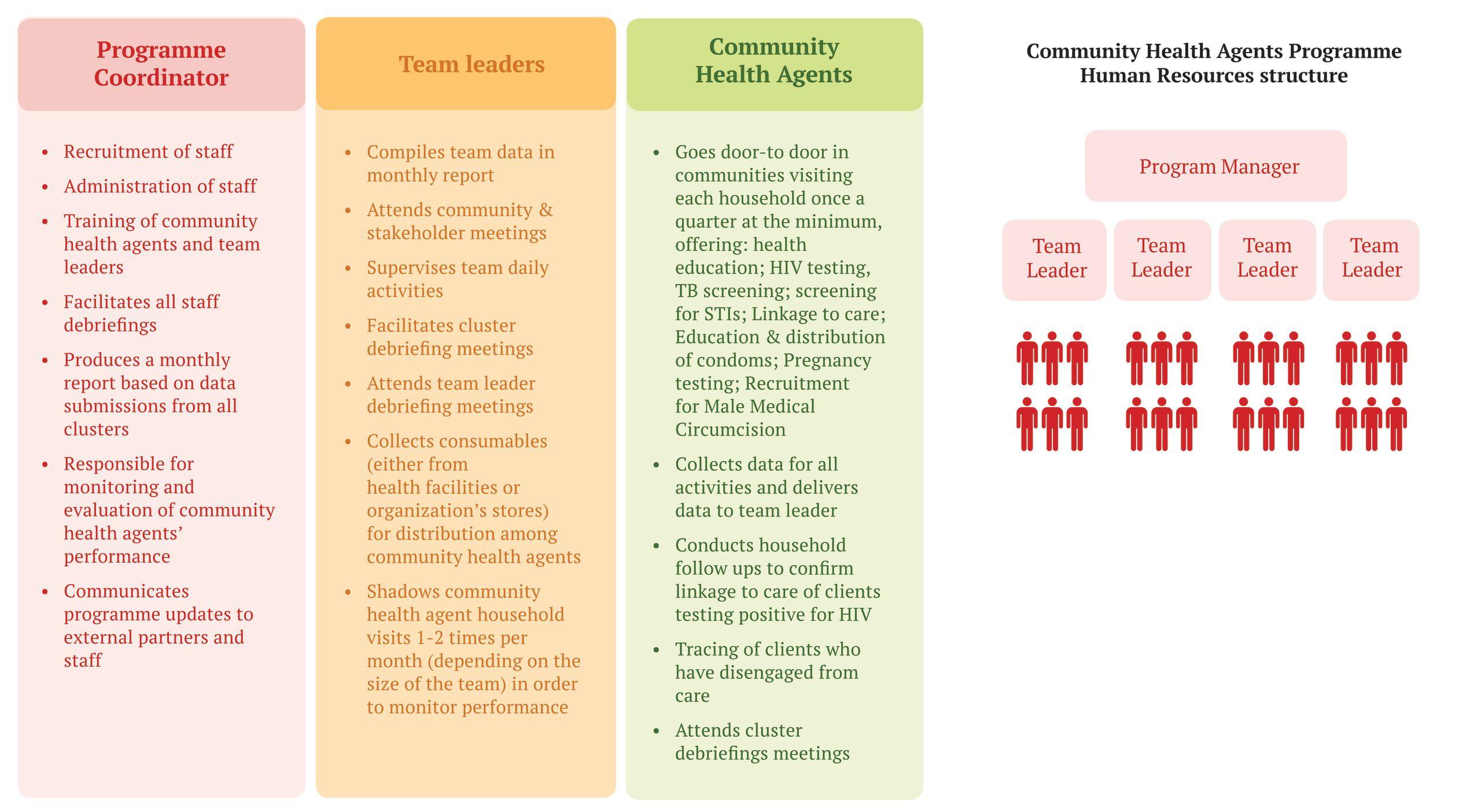
MSF experience: A team-based approach
30 community health agents were initially employed to work in the programme, each covering an area roughly within a two-kilometre radius of their own home. Community health agents were divided into teams, each team supervised and supported by a leader who served as the link with the programme coordinator. A team approach was adopted because it is easier to cover a large geographical area this way, and it meant that only team leaders need to report to health facilities, thereby minimizing the pressure on facilities. In time the number of community health agents grew to 86, divided into teams of 10-15, depending on the geographic area to be covered.
MSF Experience – Due to security concerns community health agents work in pairs in some areas; working in pairs also had an unforeseen benefit, as sometimes occupants preferred one community health agent over the other.
Roles and responsibilities in 2018 were as follows:
2.2: Develop Job Descriptions
Ensuring that job descriptions are properly worded and strategically advertised is key. MSF strongly recommends the following steps:
- When advertising community health agent posts ensure that the advertised job descriptions adhere closely to the language used by the DoH to describe this cadre of health worker if an official definition exists. In the South African context community, health agents are officially referred to as Community Health Workers, a term that encompasses ‘any worker who is selected, trained and works in the community. They are the first line of support between the community and various health and social development services. They empower community members to make informed choices about their health and psychosocial wellbeing and provide ongoing care and support to individuals and families who are vulnerable due to chronic illness and indigent living circumstances.’ [Reference]
- Salary levels for community health agents and team leaders should be drawn from the local salary grid. It is important to standardize salaries, as misalignment could make the intervention unsustainable, and foster resentment between community health workers employed in the private and public sectors
MSF experience: policy gaps continue to hamper effective deployment of CHWs
Aligning health agents’ salaries with the public sector benchmark was a major challenge for MSF, as HIV Counselling & Testing (HCT) was not then included in the scope of work for CHWs. MSF lobbied successfully for the inclusion of HCT in the scope of work for CHWs. CHW’s scope of work is now specified in the WBOT policy framework [Reference]. Following the introduction of a national minimum wage in South Africa, of R3,500 (2019 USD = $243) this is typically the starting wage for a community health worker in South Africa.
Agente Communitário de Saúde Brazil
The term Community Health Agent used by MSF is borrowed from the Brazilian context, where community health agent (agente comunitário de saúde) was the title given to a specific lay health care worker developed in Brazil in 1991 as part of the construction of the Brazilian Unified Health System established by Constitutional rule in 1988. The agent, which was said to be inspired by the barefoot doctors programme in China, is not certified to practice medicine or nursing but has the primary task of gathering information on the health status of a small community by means of a close relationship with it.
In the initial design, the agent should be one of the residents of a street, neighbourhood or surrounding region, and was to be selected on the basis of a good relationship with his neighbours, in addition to the ability to devote eight hours a day to the work. Every agent is supervised by a doctor or nurse of the health clinic, and home visits are conducted in the coverage area of a basic health unit, thus producing information that can assess the main health problems of his community.

2.3: Recruitment
To drive the recruitment process the following actions can be taken:
- Identify the best local platforms on which to place advertisements – areas of high foot traffic, such as kiosks, transport hubs, community gathering areas, etc.
- During interviews, ensure that the interviewee is from the area in which they will be working
- Involve local authorities in the recruitment process
- Be sure that successful candidates collectively are a good mix of male and female, as men particularly are more comfortable being tested by men
MSF experience: Postering trees and hiring local
- MSF advertised community health agent positions by putting posters up in high traffic areas within communities, including bus stops, shops, community halls, and sometimes trees used for community gatherings. Local authorities assisted by making announcements during community meetings, and or traditional court sessions/gatherings
- The minimum education requirement imposed by MSF was successful completion of secondary school education, with applicants needing to produce the relevant qualification certificate, known in South Africa as a ‘Matric’ certificate
- Community Health Agents were drawn from areas targeted by the programme, in consultation with traditional leaders and/or ward councillors. Applicants were required to submit a letter from a traditional leader confirming that they are known and respected in their community. Traditional leaders assisted with advertising positions, and with shortlisting candidates

2.4: Develop Guidance Tools
The following resources will provide staff - both community health agents and their team leaders - with detailed guidance on how to tackle every aspect of their work:
- Standard Operating Procedures describing every step community health agents must take when conducting household visits and doing other routine duties, such as data collection, waste management, ordering of stock, and more (See example SOP in Tools)
- Supervision tools that assist team leaders in their management of community health agents. Tools should provide guidance on how to evaluate performance, covering the manner in which community health agents introduce themselves and their work to community members; how services like health education sessions and HCT are delivered, and more (See example Supervision Tools in Tools)
2.5: Produce uniforms and necessary equipment
MSF procured the following for community health agents:
- Branded uniforms
- Identification tags
- Raincoat and umbrella for wet conditions
- A backpack containing the following necessary consumables:
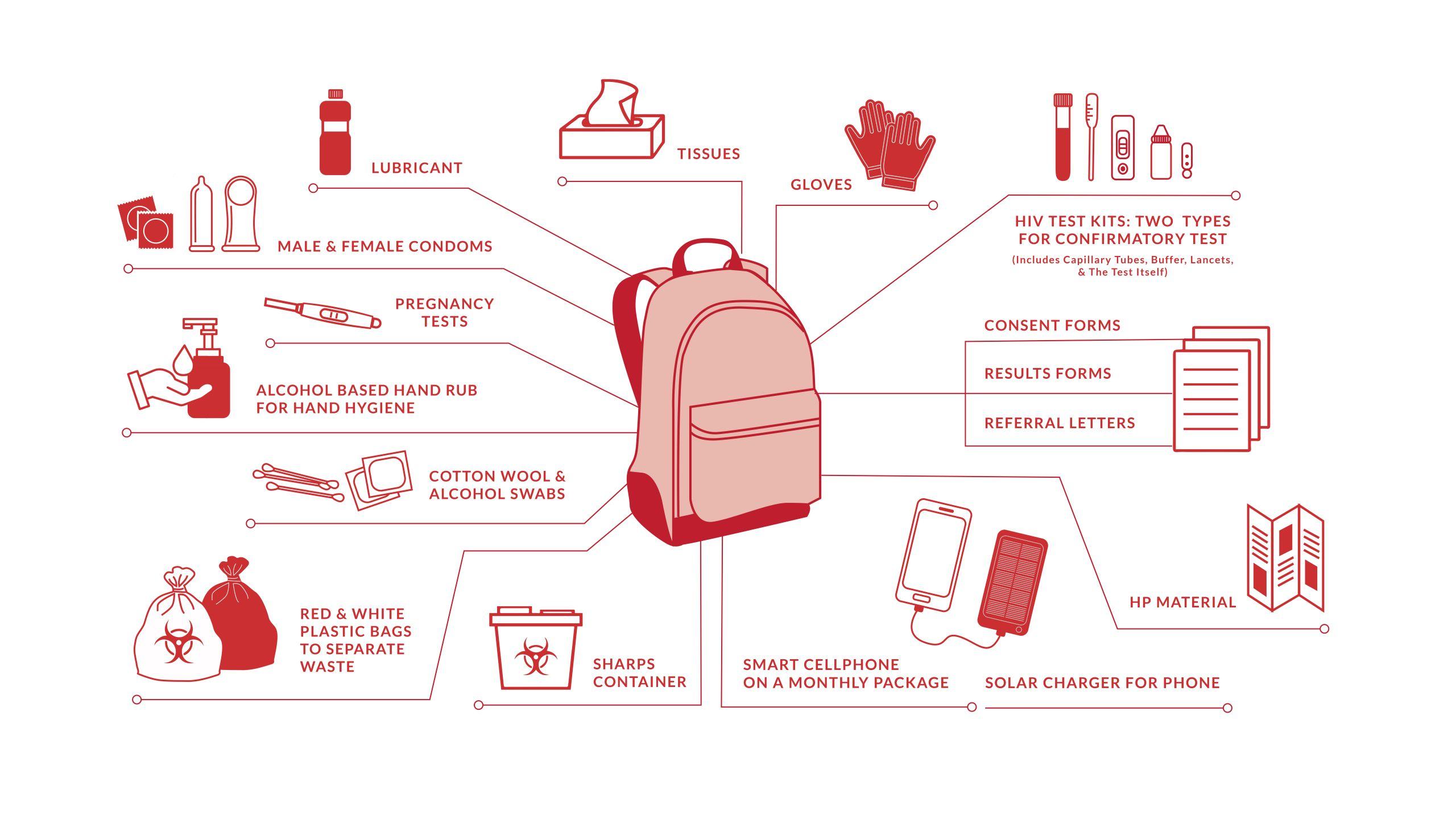
MSF Experience: A well-stocked, fit-for-purpose back pack
Experience led to tweaks in the backpack inventory over time. Given that the operational area was rural and many homesteads are not electrified, normal cellphone chargers were often useless. MSF, therefore, procured solar-powered charging devices for the community health agents, and these worked well. The type of backpack used also changed over time, as in 2017 a change in the type of HIV testing kits used required backpacks to have a cooler compartment.
2.6: Training and mentorship of Community Health Agents
To train effective community health workers, the following steps can be taken:
- Prepare training modules and materials covering all aspects of the role (examples can be found in the tools)
- Training modules should comply with local requirements to ensure the participants can receive valid certification for their course
- Establish how long the mentorship period should be, and what methodology to follow
MSF experience: Investment in training, mentorship and team spirit!
Investing time upfront in proper recruitment, training, and mentoring of community health agents and team leaders was the key to a successful outreach testing programme. The National Department of Health training on HCT for CHWs runs over 10 days, however, MSF Community Health Agents underwent a two week-long initial training, even if they had already done the DoH training. This was to ensure consistency.
Recruits were then mentored by a team leader or another experienced community health agent for a further two weeks. All community health worker programmes experience a high turnover of staff as CHW’s take on other posts; Continual trainings, including refresher trainings, are vital for success.
At the end of the mentorship period a graduation ceremony was organized by MSF, attended by local authorities, at which graduating community health agents received certificates. The ceremony recognized the efforts of new recruits, contributing to team spirit, and local authorities were able to witness skills development in action.
Step 3: Activation
At the end of the mentorship period a graduation ceremony was organized by MSF, attended by local authorities, at which graduating community health agents received certificates. The ceremony recognized the efforts of new recruits, contributing to team spirit, and local authorities were able to witness skills development in action.
3.1: Community awareness and health promotion
- Start by informing households that health agents will periodically be visiting. Explain the thinking behind the programme, and what services community members can access through community health agents; This was done through mobilisation, community meetings, Imbizos (community dialouge), training traditional leaders, training traditional health practitioners and radio slots which advertise services and provide an opportunity for health education
- Emphasize that the programme is conducted with the permission of local authorities
- Emphasize that these services are free of charge
- Emphasize that test results are confidential
- Stress the benefits of regular testing
MSF experience:
It took much longer to get into some wards than others. Accessing communities, especially people’s houses, takes persistence and patience! Having community health agents work in pairs was part of the solution, and certain wards required more attention in the form of community meetings than others. Community members were extremely concerned about the protection of their data, especially if they knew the community health agent as a ‘neighbour’ first and foremost. MSF conducted community dialogues, sometimes using theatre pieces to explain the programme, medical ethics and confidentiality of information. These dramas were very successful in alleviating people’s concerns.

3.2: Start offering services
- An introductory explanation of the programme is critical – take time to do this well!
- The introduction should be followed by a health education session and other screening services (TB & STI)
- Every person who then consents to receive an HIV test must first sign a consent form
- Testing should be offered in a room that guarantees confidentiality
- Whilst the HIV test is running, the community health agent starts preparing the patient for the result
MSF experience:
A time and motion study conducted by MSF in 2017 showed that the ‘welcome’ and ‘introduction’ activities took up 5% of the visit, and health education 20%. Taking time to do this at the pace of the householder is important as it sets the scene for the testing and screening that follows.
People are often nervous about testing in front of their family members, and HIV tests should be conducted in a spare room, ensuring confidentiality for the individual concerned. If there is no spare room, the test can be conducted outside, away from other people. In this setting it was acceptable to conduct testing under a tree outside, or in another cottage in the compound.

3.3: Referral & Linkage
- If a client tests positive for HIV it is essential that a post-test counselling session be conducted
- Information on antiretroviral treatment must be shared
- The client must be referred to the nearest clinic – to do this the community health agent must fill out a referral form
- The Community Health Agent should return for a follow up visit after 2-3 weeks to confirm linkage to care. Clients in possession of medication, or a clinic card, are considered to have been linked to care
MSF experience: Referral and linkage challenges
In 2018, MSF carried out an HIV Prevalence Survey in the Eshowe and Mbongolwane areas, and established that 94% of those who know their HIV+ status are on antiretroviral treatment. There were certainly challenges along the way, though. A major challenge was the use of different names by clients. ‘For example,’ says Patient Support Manager Ntombi Gcwensa, ‘most people know me as Ntombi Gcwensa, and if a health agent asked for my name to go on the referral form this is the name I might give, but when I go to the clinic I will use the name in my ID document, which is Immaculate Gwensa.
When it comes to MSF following up on linkage there is no Ntombi Gcwensa on record, and therefore no telling whether Ntombi Gcwensa has been linked to care!’ A correctly filled out referral form is essential for health facility staff to be able to initiate a client on treatment. If a client does not have a referral form, or if the referral form information does not match the client’s clinic records, health facility staff will offer to perform another test. However, the client might not have the time to take another test, or might not want to. To address these issues MSF health agents began asking clients to show their ID documents, to ensure that the name on the referral form matches facility records.
However, it is important to note that not all people are able to produce an ID, and this should not be a pre-requisite for conducting an HIV Test. Undocumented migrants, and/or people born in some remote rural areas do not have official documentation, and experience challenges in accessing health care. It is important that Community Health Workers are able to access all members of the community, not just those who can provide identification.

3.4: Supervision
The supervisory duties of the team leaders include the following:
- Collection of consumables (either from health facilities or organization’s stores) for distribution among community health agents
- Shadowing of community health agent household visits 1-2 times per month (depending on the size of the team) in order to monitor performance
- Team leaders should use supervision & mentoring checklist and should provide immediate feedback to their team members
MSF Experience:
MSF Experience: Hands-on supervision is the key to running a good community programme. Community Health Workers spend long hours working independently of the public health care system and its facilities. Regular debriefing sessions and refresher trainings are essential, as is continual supervision and mentoring, to ensure a good team spirit and professionalism.

3.5: Waste management
It is important that partners agree on a procedure for the disposal of medical waste, either choosing to return waste to the clinic directly or via the team leader.
MSF Experience:
Only 1-2% of MSF community health agents returned medical waste to facilities themselves, and they were those who lived in close proximity to a health facility. Others gave their waste to a team leader and/or to the supervisor for depositing with a local health facility.
3.6: Ongoing interaction with community
Without the involvement and support of communities, a door-to-door testing programme is not possible. To ensure ongoing support from communities, the following actions are recommended:
- Have regular meetings with community leaders and representatives to give and get feedback on the programme
- Discuss challenges with community leaders and representatives and agree on solutions
- Be sure to notify the community of any changes to the programme
- Consider forming a Community Advisory Board, holding regular (bi-annual) meetings to present information on activities, and to provide a space for feedback to the project from the community
MSF experience:
Izimbizo is a Nguni term describing gatherings of specific community groupings, with the aim of passing on important information or drawing community feedback on crucial issues. Imbizo can only be called by Inkosi or senior traditional leaders. In most cases, the elders, the warriors, the teens and women are called separately. Today, Izimbizo are also used for the discussion and resolution of health-related issues.
Members of rural communities respect the call from the office of Inkosi, and attend Izimbizo to listen to what their Inkosi is bringing, or seeking from them. MSF collaborated with traditional leadership and utilized the Izimbizo platform, advancing the mission of marketing the services, and expanding access to HIV Testing and TB screening, for everyone, as well as education platforms.

Step 4: Monitoring and Evaluation
Rigorous monitoring and evaluation processes are an essential part of maintaining consistent, high-quality door-to-door services. It is important that the chosen data collection system is easy for community health agents to use. It is equally important that data is analysed to determine whether or not the programme targets are realistic, or need to be revised. MSF recommends the following approach:
4.1: Data Collection
- Community health agents to make sure that every activity and every service delivered is recorded on the standardized data collection sheet, (an example of which is available in Tools)
- The data collection sheet is submitted to team leaders at the end of each week or month, depending upon volume and/or location
- Confidentiality is important – community health agents ensure that data collection sheets are securely stored until handed over to the team leader
- Team leaders compile the data from all data collection sheets and submit it to the programme manager
- Programme manager analyses data
- Reporting on the activities is submitted to the Department of Health on a monthly basis; or as required by the DOH
MSF experience: Digital data collection
MSF designed a digital mobile data collection tool in collaboration with Jembi Health Systems, the aim being to minimise paper records and to ensure efficient and immediate recording of data. The ‘CHAP APP’, as it came to be known, enabled community health agents to record both geographic and client data, and provided users with step by step guidance on the HIV testing process. The CHAP APP was uploaded onto a Samsung Pocket Neo touch-screen phone (4GB, 512 MB RAM. Weight 100.5g) and was designed to be usable both on and offline. The app automatically sent data to a database maintained by Jembi, which is compliant with South Africa’s Protection of Personal Information Act. Access to the CHAP APP was password-protected, and all data on the phone was stored in an encrypted format. Phones could also be wiped remotely in case of theft or loss.
There were some challenges experienced in using the Chap App. Community Health Agents initially reported that the app had too many pages and information fields, and was simplified into a slightly more user-friendly version in 2018.

4.2: Monitoring and Evaluation
The following is recommended for effective monitoring:
- Data should be analysed in order to track the performance of staff relative to programme targets
- Data should be analysed to work out the geographical coverage of the door-to-door testing intervention
- To ensure that community health agents are encouraged to perform and held to a standard, monitoring and evaluation information should be shared with relevant authorities, and with the community health agents themselves
Based on what the data analysis reveals some modification of the programme might be necessary:
- Routine analysis of programme data by the programme manager will indicate whether modification is needed
- Signs that the programme might need to be modified include disproportionate testing coverage between age groups, and between the sexes
MSF experience: modification
MSF modified the programme significantly over time. For example, working days were changed from Monday-Friday to Tuesday-Saturday, in order to reach those who work during the week. According to MSF Patient Support Manager Ntombi Gcwensa, ‘When data analysis began to show that community health agents were testing mainly grannies and babies, our site coverage was expanded to include shops and community gathering points’. Various additional services including recruitment for male medical circumcision were added to the service offering over time.

Evidence
The Community Health Agents Programme as part of a comprehensive testing and counselling package
Evidence
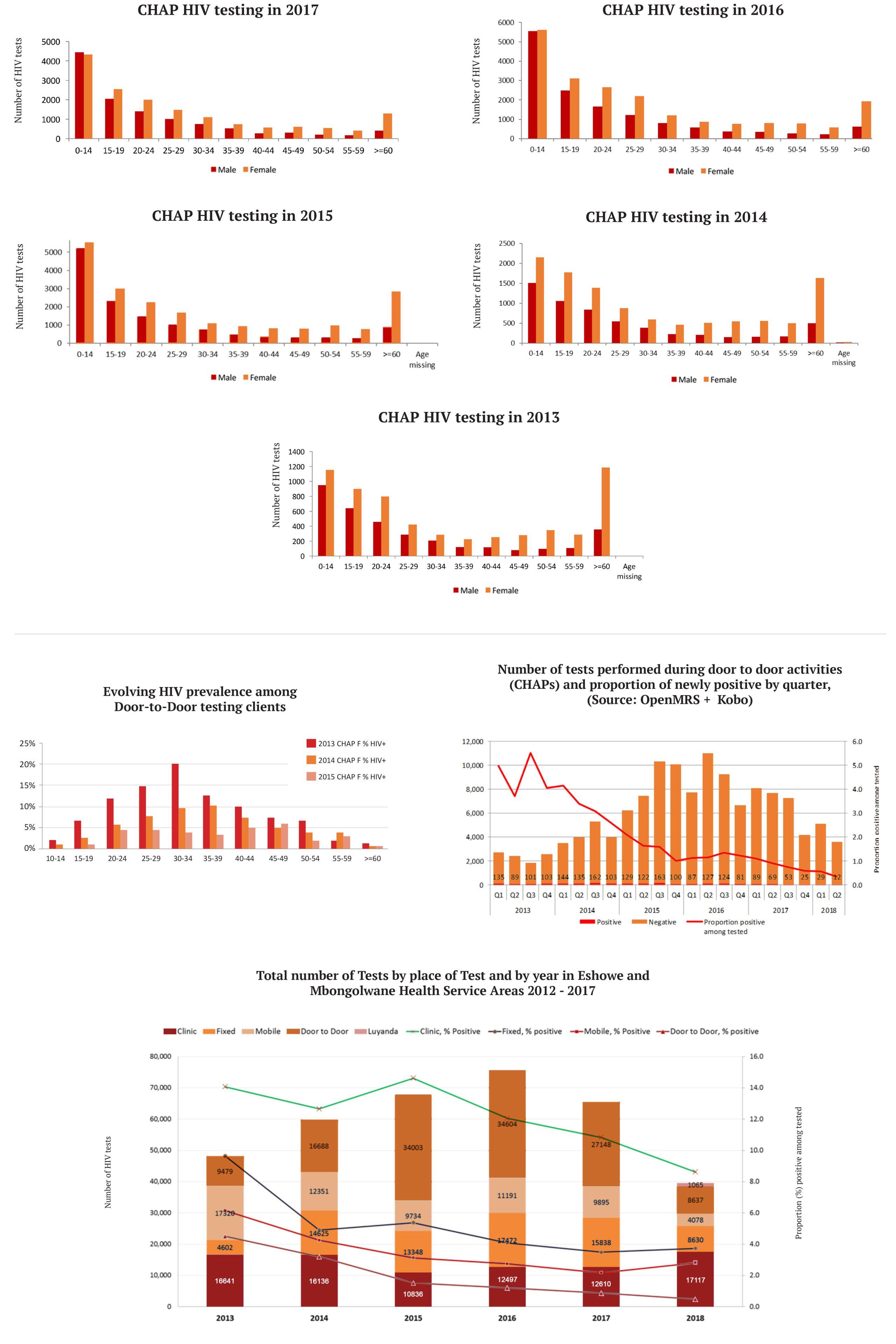
The MSF Community Health Agents Programme was part of a comprehensive testing and counselling package, which included fixed testing sites (testing sites within communities, outside of primary health care facilities), a mobile van, testing tents and facility-based testing. Door-to-door testing conducted by community health agents yielded a lower proportion of HIV positive individuals than other testing interventions (refer to the graph below).
It is likely that at the start of the programme, many clients were offered testing for the first time, or after a long inter-test interval, contributing to the relatively high positivity rate (between 4-6% in 2013/2014). It is likely that over time most of the accessible HIV+ population was identified, leaving a relatively lower-risk population being regularly retested, and yielding relatively few new HIV+ diagnoses.
A 2016 study of the demographic reach of community HIV testing in rural KwaZulu-Natal found that Door-to-Door testing covers most adult sex-age strata except men 15-29 years, and demonstrated that repeated offers of HIV testing leave fewer and fewer undiagnosed HIV+ clients, a phenomenon known as ‘saturation of testing’.
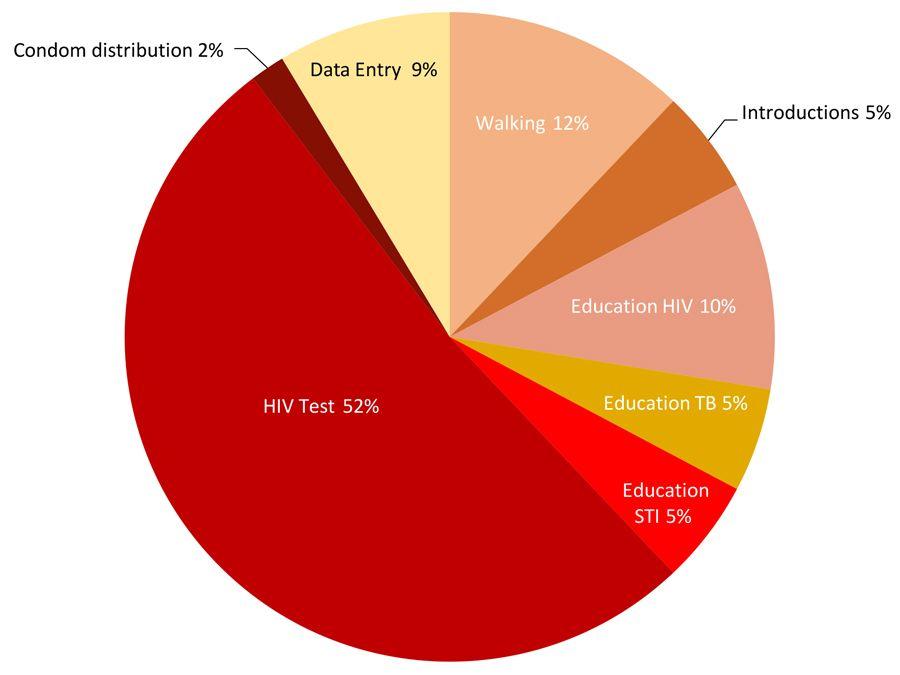
An MSF ‘time and motion’ study conducted in November 2017 showed that each homestead visit by a community health agent, or pair of community health agents, took an hour on average. Testing accounted for the bulk of time spent at each household. Walking between homesteads also took considerable time.
Time & Motions Study: Division of the time between activities

Costs
Important to establish the comparative costs and benefits of the different testing strategies.
In the context of an HIV incidence reduction project such as the “Bending the Curves” project MSF established in King Cetshwayo District it was important to establish the comparative costs and benefits of the different testing strategies.
An evaluation of the community testing modalities was conducted in December 2015, analyzing HCT data from early 2013 until November 2015.
The study concludes that:
Community testing models may offer better access to some difficult-to-reach groups, and the Door-to-Door Programme per HIV- & HIV+ test cost was the least costly modality for community HIV testing.

Lessons Learned & Recommendations
In the five year life term of the Community Health Agents Programme the following key lessons were learned
Bending the curves of the HIV epidemic requires placing individual choice and patient-friendly options at the centre of programme strategies. The experience of MSF and the KZN DOH in King Cetshwayo District, at the heart of the epidemic, has demonstrated the feasibility and acceptability of a wide range of strategies, including a door-to-door HIV testing programme called the Community Health Agents Programme, that increased the number of people initiated on treatment, and provided the support they needed to reach viral suppression.
In the five-year life term of the Community Health Agents Programme the following key lessons were learned:
1. Door-to-door testing is essential
MSF is of the firm opinion that its success in reaching the UN 90-90-90 by 2020 targets and achieving 90-94-95 two years ahead of time, is due in part to the comprehensive nature of its HCT programme, including door-to-door testing, and the subsequent linkage to care activities conducted by the community health agents.
It is also important to recognize that community-based testing models have the potential, through education, to catalyze behaviour change in those who test negative for HIV. Community-based models of testing are also a valuable vehicle of referral to other health services.
2. Ensure that community health agents or CHWs represent a mix of sexes and age groups
It is particularly important to ensure that there are males in the complement of door-to-door testing teams, as men are not always comfortable being tested by women. It is also vital that there should be a generational mix, as MSF found that some young individuals were not comfortable being tested by their peers.
3. Stringent Monitoring and Evaluation required
MSF struggled with thorough documentation of its door-to-door programme, with the consequence that linkage to care was difficult to document. MSF evaluated linkage to care on a quarterly basis but on reflection MSF strongly recommends that linkage to care be evaluated in real-time; that is, for each person found to be HIV positive or screened positive for TB, to be linked to care immediately, and documented as such.
4. After the initial intervention, door-to-door testing should be periodic rather than constant
Over the five year span of the programme the proportion of those testing positive for HIV fell dramatically, as did the number of tests in general, and testing became concentrated among the very young and the very old. For these reasons, MSF and the DoH shifted focus to rural fixed sites, which are based in key social intersections in rural areas, for example by shops, or at crossways.
These rural fixed sites have been shown to attract a more even spread of men and women from a greater range of age groups. MSF’s recommendation is that door-to-door testing is revived every 2-3 years for a period of between 3-6-12 months, depending on the location.

Tools
Downloadable Forms

Checklist
Downloadable Forms

Training Materials 2013/2014
Downloadable Forms

Training Materials 2016
Downloadable File

Training Materials 2019
Downloadable Files

Job Description
Downloadable files

Budget
Downloadable file
Contact

For Operational Feedback and Support, contact Support Manager in Eshowe Ntombi Gcwensa, MSF Patient, email: MSFOCB-eshowe-htc@brussels.msf.org
For media or page-related queries, contact MSF Field Communications Manager Sean Christie, email: MSFOCB-Capetown-ComsOff@brussels.msf.org

Acknowledgements
Recognition
Our sincere gratitude goes to the respective Traditional Authorities who embraced the community health program and assisted us in turning an idea into reality.
We would like to thank our partners, the Department of Health of Kwazulu-Natal and in particular, the District Health Offices of King Cetshwayo, SHINE, Child Care SA, and uMlalazi Municipality as well as all community members that were involved in supporting the programme.
Finally, acknowledgement is due to all the Community Health Agents who have been courageously running kilometres to provide quality services for their population and made the success of this program.
(Cover photo: A Community Health Agent in a household visit. © Peter Ceaser)




