In 2015, South Africa started implementing ‘Option B+’ for HIV-positive pregnant women, offering them antiretroviral therapy for life regardless of CD4 count. Subsequently, mother-to-child transmission (MTCT) of HIV in South Africa has fallen from 16,000 (2010) to 5,100 (2015) new vertical infections annually [1]. Despite this success, some challenges remain, including relatively high postnatal transmission, estimated to be around 4.3% when infants reach 18 months of age [2].
Khayelitsha is a township on the outskirts of Cape Town, with a total population estimated at 500,000-1,000,000 people. The HIV antenatal prevalence is high (about 30%) compared to the rest of the Western Cape Province (5%) [3]. In 2013, 98% of pregnant women were tested for HIV on the same day as their first antenatal visit and started on antiretroviral viral treatment (ART) as a result of integrated antenatal care and HIV care[4]. At 10 weeks of age, MTCT is estimated at 0.8%[4]. However, there is no data on the MTCT rate at 18 months due to poor test uptake--about 30% of exposed infants return for 18-month testing[4].

Studies have suggested that adherence to ART may be lower among postpartum women compared to non-pregnant adults started on ART[5][6]. There is also mounting evidence that postpartum retention in care of new mothers is poor. A study in the nearby township of Gugulethu suggested that nearly 30% of mothers default on ART in the first six months after delivery[6].
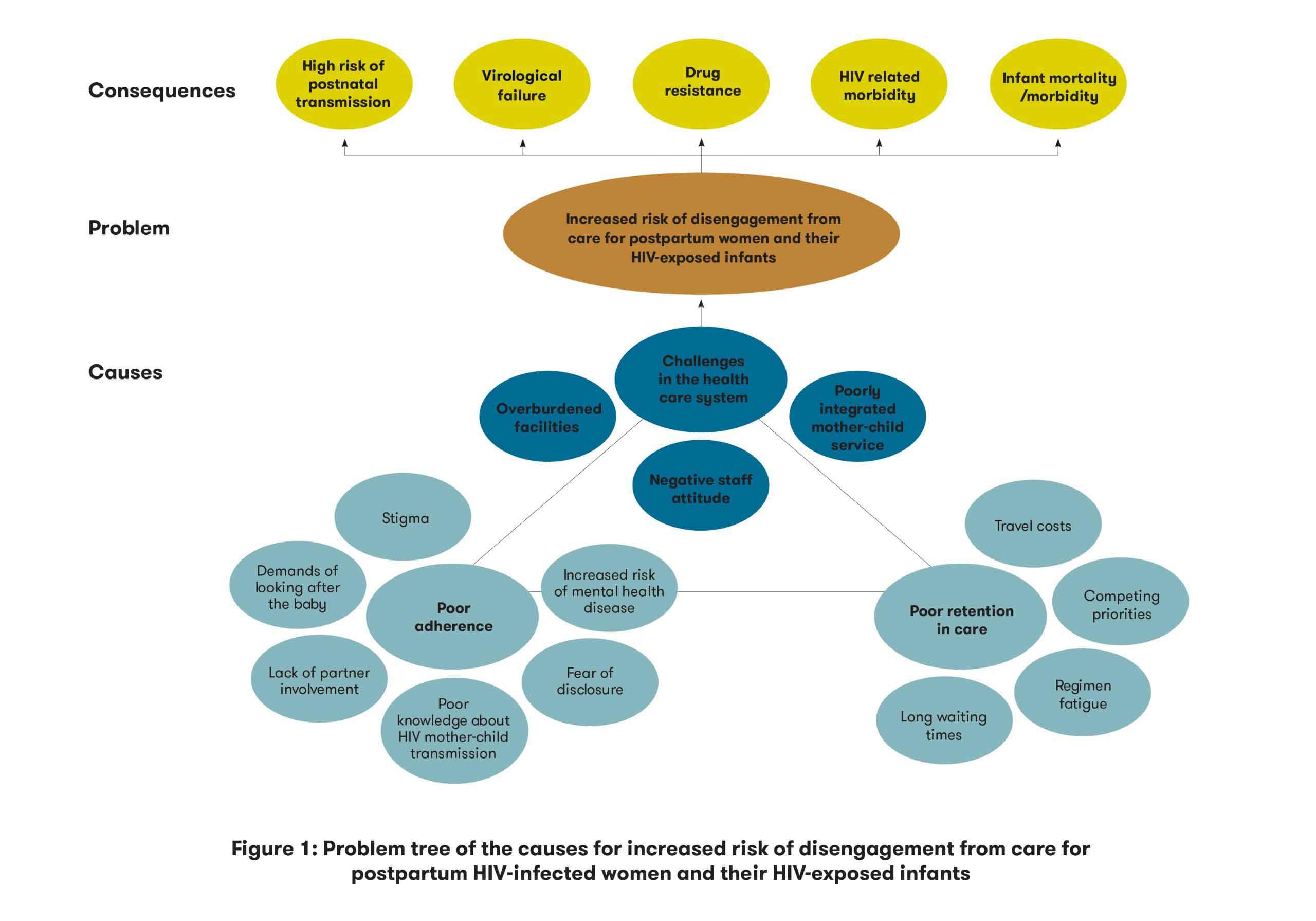
Non-adherence leads to viral rebound and an increased risk of postpartum MTCT through breastfeeding. Reasons for poor maternal retention in care are summarized in Figure 1 and are thought to include: long waiting times and high patient volumes at the antiretroviral (ARV) clinic, younger maternal age, non-disclosure of HIV status, travel costs, inadequate knowledge about postnatal MTCT, stigma, regimen fatigue, and lack of partner involvement[4] [5] [6] [7].
Furthermore, the literature suggests post-delivery responsibilities including stresses and demands of caring for a newborn may be a potential barrier for adherence to treatment[8]. Also, negative staff attitude is considered to be a reason for declining retention in care rate among pregnant and postpartum women[6][9].
Studies have suggested that adherence to ART may be lower among postpartum women compared to non-pregnant adults started on ART. There is also mounting evidence that postpartum retention in the care of new mothers is poor. A study in the nearby township of Gugulethu suggested that nearly 30% of mothers default on ART in the first six months after delivery.

Non-adherence leads to viral rebound and an increased risk of postpartum MTCT through breastfeeding. Reasons for poor maternal retention in care are summarized in Figure 1 and are thought to include: long waiting times and high patient volumes at the antiretroviral (ARV) clinic, younger maternal age, non-disclosure of HIV status, travel costs, inadequate knowledge about postnatal MTCT, stigma, regimen fatigue, and lack of partner involvement. Furthermore, the literature suggests post-delivery responsibilities including stresses and demands of caring for a newborn may be a potential barrier for adherence to treatment.
Also, negative staff attitude is considered to be a reason for declining retention in care rate among pregnant and postpartum women. One strategy to improve postnatal care and postpartum HIV care is an integration of services. In 2011, UNAIDS recommended the integration of prevention of mother to child transmission(PMTCT) with maternal, newborn and child health services[8]. South Africa produced a national PMTCT integrated model in 2011, recommending “integration of PMTCT into the existing maternal and child health interventions”. However, the implementation of integrated postnatal maternal and child health has been generally poor and ineffective.
In recent years, adherence clubs have been adopted in South Africa as a differentiated model of care for clinically stable adults on ART. Adherence clubs serve the dual purpose of decongesting health facilities by scheduling group prescription pick-up of ART and health checks and also provide an environment of peer support to patients on ART. Clubs have shown good patient retention in care and virological outcomes compared to standard of care[10][11]. Different models of clubs have since been assessed, such as community-based adherence clubs, which also showed good adherence and retention in care[12].
Following lessons learnt from implementing adult adherence clubs, Doctors Without Borders (MSF) in partnership with mothers2mothers (m2m) and City of Cape Town (CoCT) Health decided to create a new differentiated model of care called “Postnatal Clubs” (PNC). The objective of the toolkit entails:
What is the purpose of this toolkit?
The objective of the toolkit entails:
- To provide programmatic information and advice on what is required to start PNCs in other facilities.
- To provide a practical guide implementing and managing PNCs to assisting the health care staff in supporting mother-infant pairs (MIPs) in clinical care and early childhood development (ECD) as part of First Thousand Days.
Introducing Postnatal Clubs

What is a Post-Natal Club?
Post Natal Clubs/PNC is a holistic patient-centred model of care addressing the medical needs of both a mother living with HIV and her HIV-exposed infant. It also provides peer support, psycho-social support and ECD support

What are the Postnatal Clubs?
Post-Natal Clubs aims
- Retention in care (RIC) of MIPs
- Maternal HIV viral load suppression
- Prevention of mother to child transmission (PMTCT) of HIV
- Infant HIV testing uptake
- Full vaccination of infant
- Improved quality of healthcare for mother and infant
Roles & Responsibilities
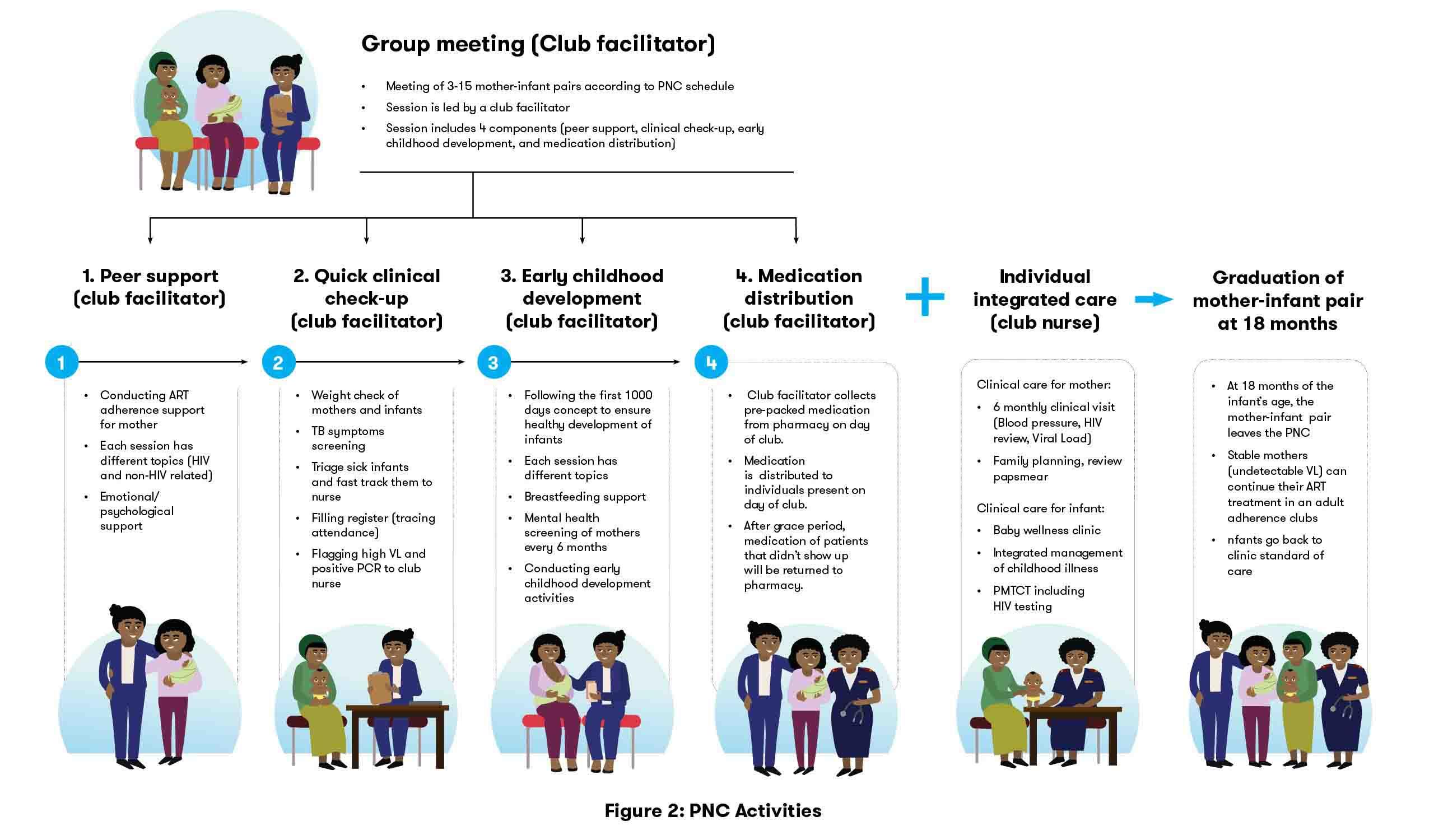
The PNC model relies on a number of different healthcare workers to run smoothly.
Figure 3 provides an overview of each staff member involved in PNCs and a detailed explanation are in the text on the next page.
They oversee the proper functioning of the clinic and allocate human resources appropriately. The FM takes responsibility for all the programmes at the facility including PNCs. Therefore, it is important to keep the FM informed about all club activities to receive adequate support when the club teams need it.
The club champion oversees the scheduling of club meetings and prescriptions at district level.
The PNC nurse is responsible for the clinical oversight of PNCs including outcomes of viral load (VL), polymerase chain reaction (PCR) tests and pap smears. The PNC nurse ensures the club team is in place and the standard operating procedures (SOPs) are followed with respect to recruitment, club preparation, club session activities, follow-up and tracing of patients, as well as monitoring and evaluation.
They prepare the prescriptions for the mothers of the PNCs. They also provide individual integrated care for HIV-positive mothers and their exposed babies including HIV and non-HIV care as well as management of childhood illnesses. For high-risk mothers of a PNC (with high VL), clinical care will be provided monthly and extra support to address risk of treatment failure will be given. They check the completeness and accuracy of the club register and keep the FM informed about the club progress.
They support the PNC nurse with regard to all clinical questions. They see all referred patients who require further review (e.g. hypertensive patient).
The PNC facilitator is usually a peer-educator, but the position could also be taken by a lay counsellor. He/she makes sure the club venue, medication and all the patients’ folders are ready for the club session. He/she recruits the HIV-positive mothers and their HIV-exposed infants into the PNC.
They are in charge of preparing the clubs and carrying out the four club component activities. Firstly, they conduct peer adherence support. Secondly, there is a weight check-up for mothers and infants as well as a TB symptoms screening. They point out high VL and positive PCR tests to the PNC nurse.
The third component entails the provision of ECD, followed by the distribution of prepacked ART. They complete the club register with all relevant data of the club visit. Every six months they administer the mental health screening questionnaire to the mothers. They trace patients who did not come to the PNC session. For “high-risk” mothers extra psychosocial support will be provided.
They ensure that prescriptions have been completed and pre-pack ART medication for club members. If a member did not attend a club session, they will take care of the medication. Uncollected parcels will be kept separate.
The clerk takes responsibility for capturing club patients’ visits into the facility’s electronic database. When all patients of the current visit are entered, the data clerk signs off on the cover page next to the current session date.
After each page of the club, register has been captured completely, the clerk signs off at the designated column indicating that all patients’ club visits have been captured. The tasks of capturing club data shall be distributed among all data clerks to ensure the timeous capturing for all data.

Programmatic Information on PNC Execution
What components are required and/or recommended to start an intervention?
Next to each component we have written required or recommended as a guide to assist with designing and planning a new PNC.
What is required below is what we think is needed for a medium clinic of between 120-250 HIV exposed babies (PMTCT babies) attending per year to form 12 clubs a year (once a month) with a maximum of 15 mother-infant pairs per club. This means that at least 70% of PMTCT babies should be in PNC for the model to work properly (as with adherence clubs, the model is otherwise too cumbersome if only a few babies are in the PNC).
It is first important to get buy-in from the department of health (DOH), both provincial and substructure, prior to the implementation of the pilot. Also prior to implementation, we recommend discussions at the clinic level with the facility manager as well as other staff to get the whole facility’s buy-in. Further discussion and workshops should be done with the team that will be implementing the PNC. Buy in from relevant community-based organizations to support the model is also recommended.
Having adequate space to see the patients is necessary for the intervention. We recommend a room where the support groups can take place where a blanket/mat can be laid on the floor for the babies to rest and interact on during the ECD components of the support group. An adjacent/close by clinical room for the nurse to consult the mother-infant pair is ideal, but a room could be “made” with separating screens and a mobile bed.
One Facility Manager is on board with the intervention and assists with human resource (HR) allocation to maximise staff potential.
One NIMARTed professional nurse who is able to deliver both maternal and child health interventions and who oversees the PNC (including preparations). We estimate that this nurse would end up spending about half of her time at the clinic on the PNCs.
One doctor is available on request to see complicated cases (for example hypertensive patient). (Light support)
One clerk to capture the PNC registers, the mother’s folders (for clinical visits or family planning interventions) and the children’s folders, as well as to assist with folder retrieval (working one-quarter of the time on PNC and preferably experienced with club batch capturing).
One pharmacy assistant to help with the pre-packing of the PNC chronic medication (working one-quarter of the time on PNC).
One pharmacist to oversee the work of the pharmacist assistant (light support).
At least one counsellor/community health worker (recommended two):
- ideally: peer HIV positive mentor mothers who are trained in PMTCT and have group facilitation skills (for example m2m mentor mothers). Alternatively could also be counsellors, community health workers, other mentor mothers
- required: group facilitation skills, experience with HIV (either living with HIV or having done previous work with people living with HIV)
- recommended: containment/coping skills, organizational skills
- recommended trainings: PMTCT, ECD, mental health screening, session guide
To gain time during the consultations, we have found that the use of integrated stationery could improve the efficiency of the model. For example, to reduce the amount of papers being filled and to prompt the nurses on what services to deliver, we have developed in collaboration with City of Cape Town integrated paediatric stationery.
We also recommend using an adapted adherence club register for time efficiency so that at each visit which is not clinical, the register can be filled rather than the maternal folder. A normal club register can also be used instead of the adapted one.
At certain clinical visits (6 monthly for the maternal VL and according to the PMTCT guidelines for infant testing), VL and PCR will be taken. It is very important to have a system in place so that these results are checked a week after they are taken. Three months could have lapsed if the results are not checked until the next club visit. For example with a high VL in a breastfeeding mother, it would be unsafe to wait three months until seeing the mother again. Systems should be in place to check VL and PCR results and to also recall the mother. We recommend:
- a designated person to follow up on VL and PCR results. Ideally every week, this person checks if any VL or PCRs were done in the clubs of the preceding week, print the results and fill them in the club register. For example, the facilitator could be in charge of this as they are responsible for the club register
- a notification system to alert the PNC nurse if there is a high VL (>50) or positive PCR result. This can be done through the printed results being shown to the PNC nurse if VL>50 or PCR positive, after some basic training on the meaning of results for the facilitator.
- a person responsible for recalling any mother with a high VL or baby with a positive PCR result. This could be the PNC nurse as she is ultimately responsible for the PNC patients. Patients should be recalled within a maximum of a month of their high VL or positive PCR result.
Half a day preparation time is required for the PNC nurse to prepare for the clubs, i.e. mostly scripting for patients in the PNC, reviewing results, etc.]
Support groups should happen at every PNC, involving all the mother-infant pairs in each group. Suggested topics are in the session guide but could be adapted to the context. Support groups can be facilitated by a peer mentor mother/counsellor/ community health worker as described above.
To facilitate the logistics and preparation around PNCs and to gain time, it is recommended to dispense the medication pre-packed (either by a pharmacy or by a chronic medication unit).
Because most of the PMTCT babies are now in the PNC, there is no need for a dedicated PMTCT nurse as there is very little PMTCT work outside the PNC (apart from recruitment). Therefore, it is recommended that more than one MCH nurses are familiar with PMTCT so that they can deliver the services on any days.
In the Western Cape, we have an intervention called Risk of Treatment Failure (ROTF), which is a local version of Enhanced Adherence Counseling. In the ROTF, the nurse provides most of the counselling herself. Through the ROTF, the high-risk mother would be seen monthly and receive monthly ARVs until she has suppressed her VL.
- Required: Scissors, string, glue, foil
- Recycled (brought in): toilet paper rolls, sticks, stones, paper plates, crayons, magazines, paper, medication bottle lids, ice-cream/yoghurt pots, margarine pot lids, newspaper, empty Lays/Simba chips bag
We recommend that the facility buys a few basic things for the ECD activities to take place. The rest will be used from recycled material, either found in the facility or brought in by the mothers/PNC facilitators. If the facility is unable to buy these items, ECD should still be taught (the concept of it) and songs/games could replace the activities described in the manual.
We recommend using the following indicators to be able to monitor how well the PNC is doing:
It would help the implementation of the PNC to have a PNC champion at the subdistrict level. This PNC champion could be the same person as the ART Adherence Club champion. His/her main responsibility would be to assist with coordinating the PNC schedule for the year for each facility having PNCs as well as ensuring that the CDU scripting cycle is working (if in use).
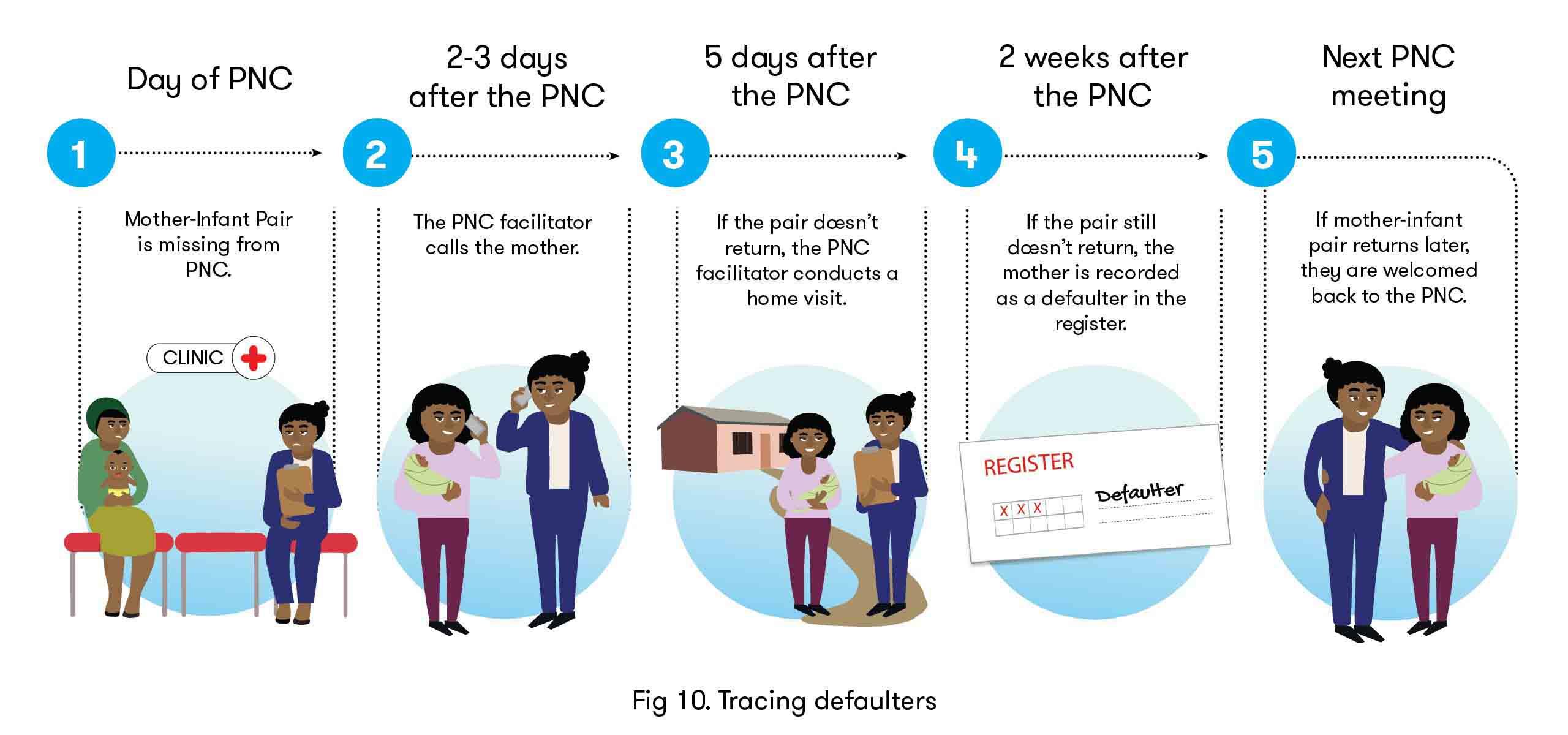
To improve retention in care and outcomes, we recommend tracing defaulting mothers. The clinic can use their usual early defaulter tracking system or trace defaulters as per the SOP 1 week after the club. We recommend that mothers defaulting visits are traced (except when a buddy comes instead of mothers- permitted at non-clinical visit for the mothers) as soon as possible, as the risk of MTCT increases if they are breastfeeding and not taking their ART.
Community health workers can do home visits to assist with the tracing of defaulters and also for high risk mothers to determine the home situation.
A cost analysis was done to calculate the additional cost to a facility when implementing the PNC model. It is based on an average clinic size of 250 new HIV-exposed babies per year. The additional cost to the facility is R1783.55 per year, which is R7.13 per infant per year. This excludes staffing and other requirements that would otherwise already be in place for the normal running of the clinic.
step-by-step-guide
A PNC consists of 3-15 MIPs and should not exceed the maximum number to ensure the emotional and psychological peer support and ECD activities can be carried out in an appropriate way.
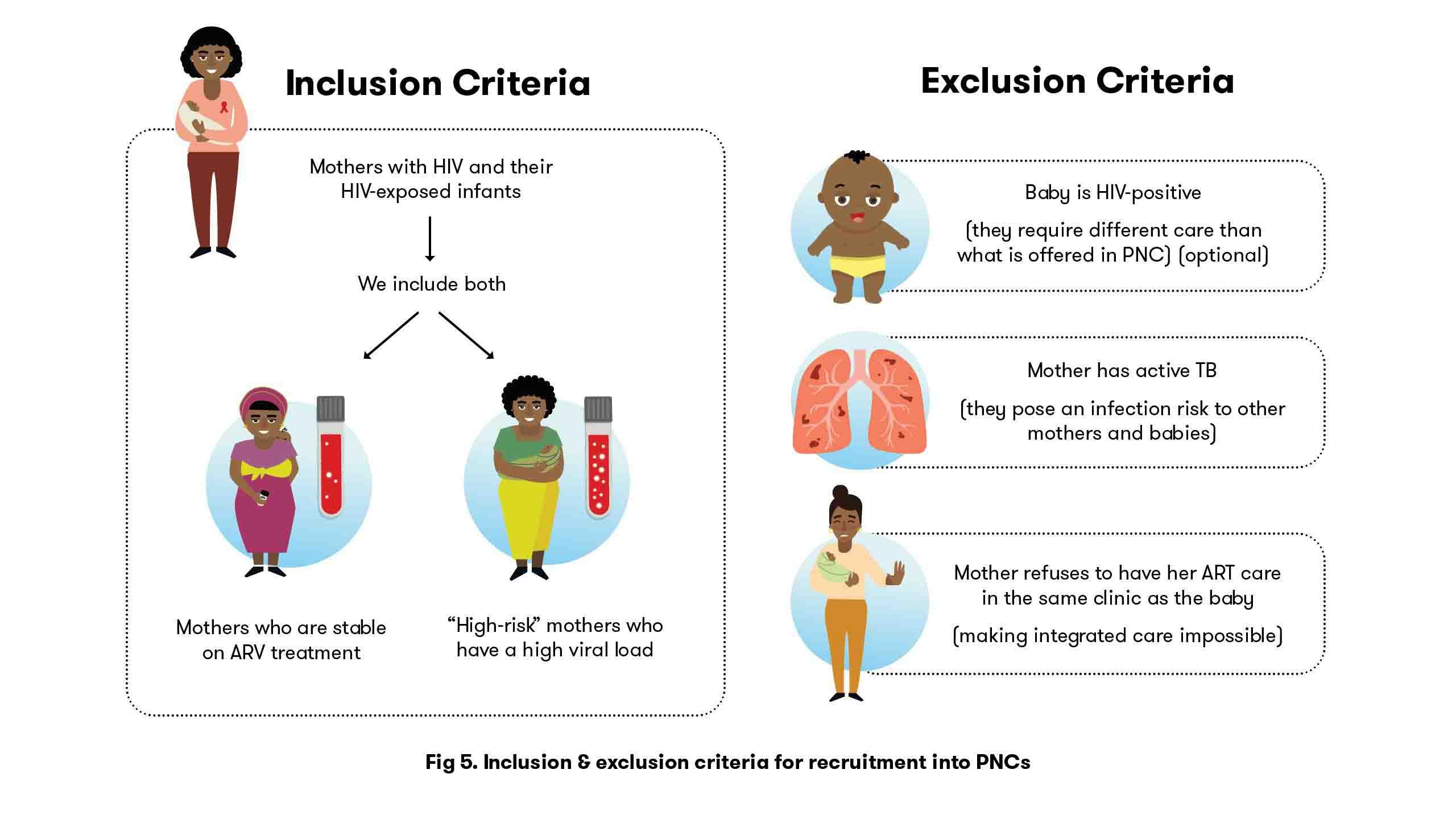
1. Who do we recruit for PNC?
Any HIV-positive mother, regardless of age, VL and drug regimen, can join a PNC with her HIV-negative infant if she wants to have integrated mother-child care.
The eligibility criteria can be adapted based on what is required and needed from the mothers and the community.
High-risk mothers
According to the South African PMTCT guidelines of 2020, a mother is considered at high risk of HIV transmission if:
- mother on ART with most recent VL>=1,000 copies/ml
- mother HIV positive but not on ART:
- newly diagnosed HIV-positive while breastfeeding
- previously diagnosed HIV-positive but not initiated on ART or discontinued ART
2. When and how do we recruit for PNC?
When the HIV-positive mother first presents to the clinic (usually at 6 weeks), she is given the option of joining a PNC and given a date and time for the first session of the PNC. However, the time of recruitment should be flexible depending on the facility and its capacity for recruitment. The recruitment is usually done either by the club facilitator or by the nurse seeing the MIP. Babies are grouped into clubs per the same month of the date of birth.
Posters about clubs and the eligibility criteria are one strategy to keep mothers informed about the PNC system. Patients who are already members of a PNC could disseminate knowledge about PNCs by word of mouth and by functioning as patient advocates. Additionally, mothers could receive information about PNCs during their pregnancy.

3. How often do clubs occur?
In the first 6 months, babies are seen monthly because of their higher mortality and morbidity risk in this time period.
After 6 months of age, clubs are held every three months until 18 months of age. These visits follow the “Road to Health” card clinical meetings. “Road to Health” is a booklet given to every newborn in South Africa which includes immunization cards, health messages, and other information relevant to early childhood development.
Download the “Road to Health” card.
Download the PNC Schedular app to assist you in making your clinic PNC schedule.
4. Preparation before a PNC
Duties or actions that are required before a club session are explained below as well as the responsible person for action.
Action and Responsible Person
Club facilitator:
- Ensure pre-packed ART medication is available at least a day before the club meeting
- Check the room is available and ready for the club meeting
- Collecting mother and infant folders
- Collecting the club register before the start of the club meeting
- Collection of pre-packed medication on the day of the club
- Ensure you have the materials required for ECD activities
- Ensure preparation of the health talk topic for each session according to the schedule
Club nurse:
- Scripts need to be issued a few days before the club meeting so that medication can be pre-packed
Pharmacist/Assistant/ CDU system:
Pre-packing ART medication a few days before the club meeting.
On arrival at the facility, mothers and babies go directly to the club room, without having to queue at the reception. The mothers’ folders, as well as their babies’ folders, are kept in separate club crates or separate shelves. The fact that a mother and her child are enrolled in the PNC is clearly identified on the mother’s and baby’s card so that their folders are easily retrievable should they come to the clinic outside the PNC.
The nurse prescribes the mother’s ARVs a few days before the PNC. The pharmacy will pre-package medication, using pharmacy stock or supplies from CDU (a central pre-packaging facility dispensing chronic medications for clients in the Western Cape). The club facilitator collects the prepacked ARVs from the pharmacy on the day of the PNC.
At the first visit, mothers are provided with an ART buffer stock of an extra two weeks, as some of the clubs are spaced more than multiples of 28 days apart.

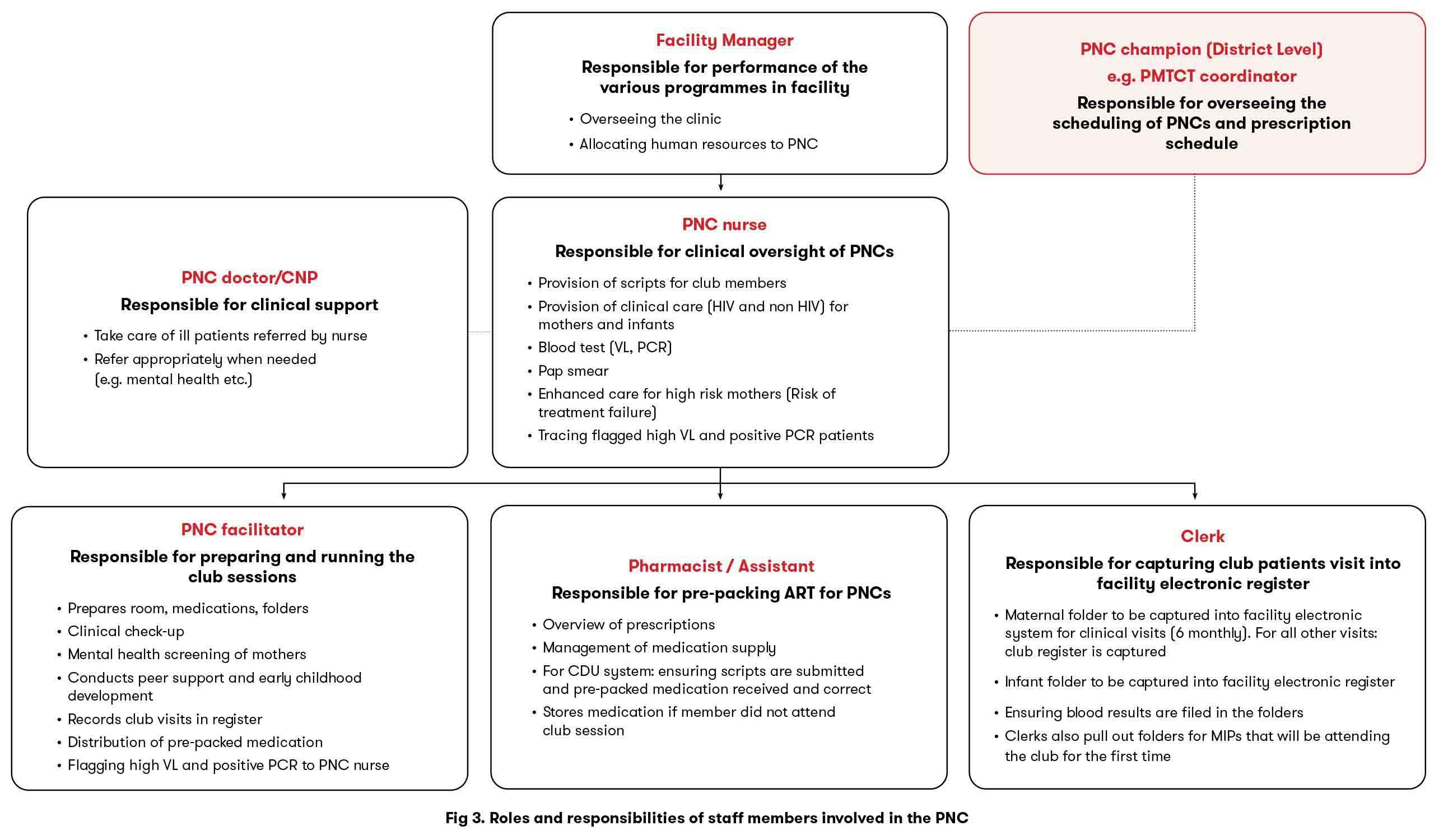
5. What happens at each club?
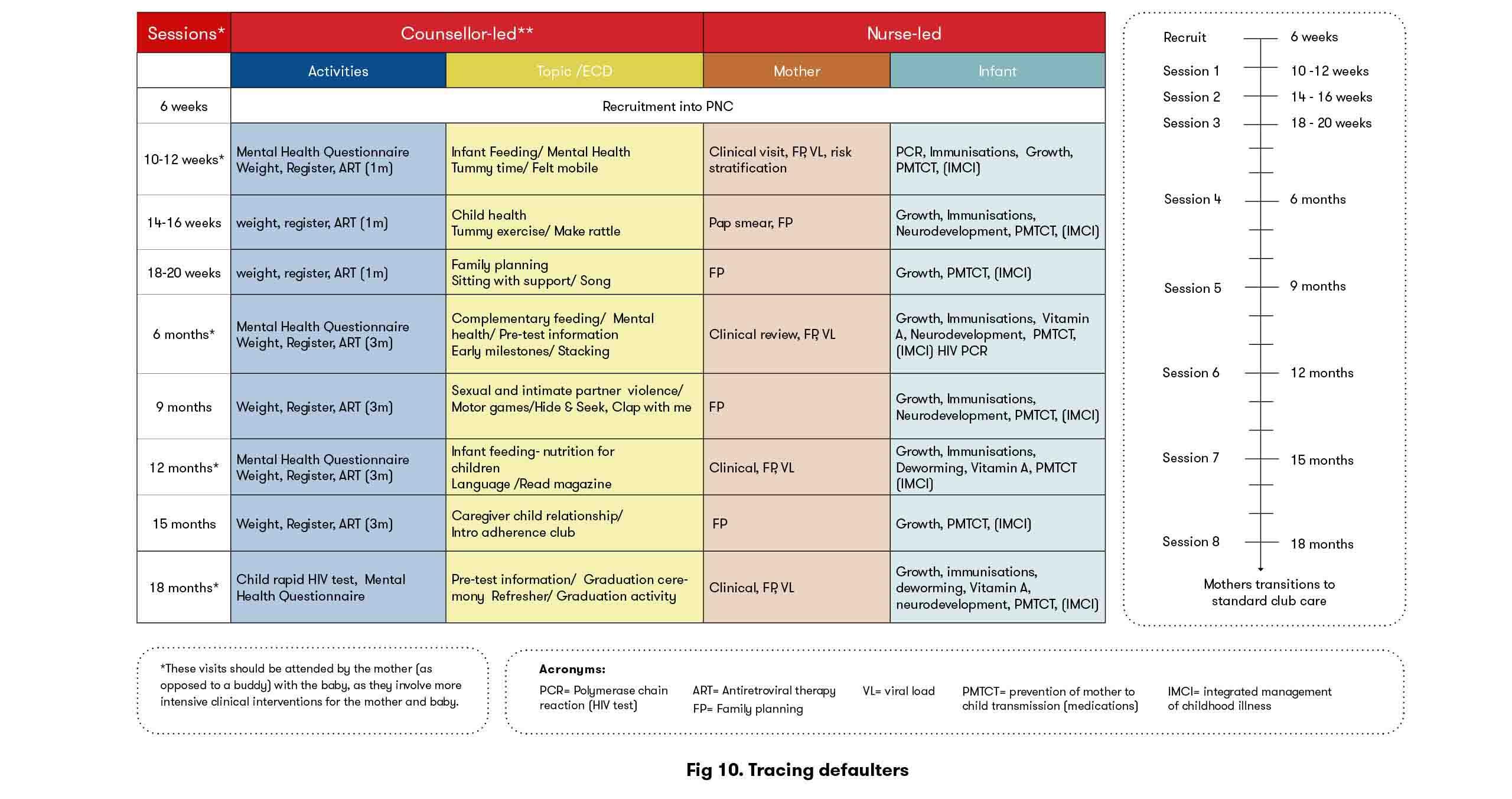
As in the adult club model, the PNC starts with a peer support session, which is led by a club facilitator. ECD activities and promoting the “First 1000 Days”/”Side by side” campaign are included. MIPs will then have a doubly integrated clinical session provided by the PNC nurse. Each visit’s interventions will depend on the age of the baby. The mother’s clinical care schedule is also adapted around the baby’s visits. To facilitate the process, integrated stationery helps map the clinical care requirements for each visit.
When the child reaches 18 months of age, the MIPs graduate from the PNC. The mother's transition as a group into an adult club, so that they keep up the peer support they created within their PNC. The babies go back to a standard of care services.
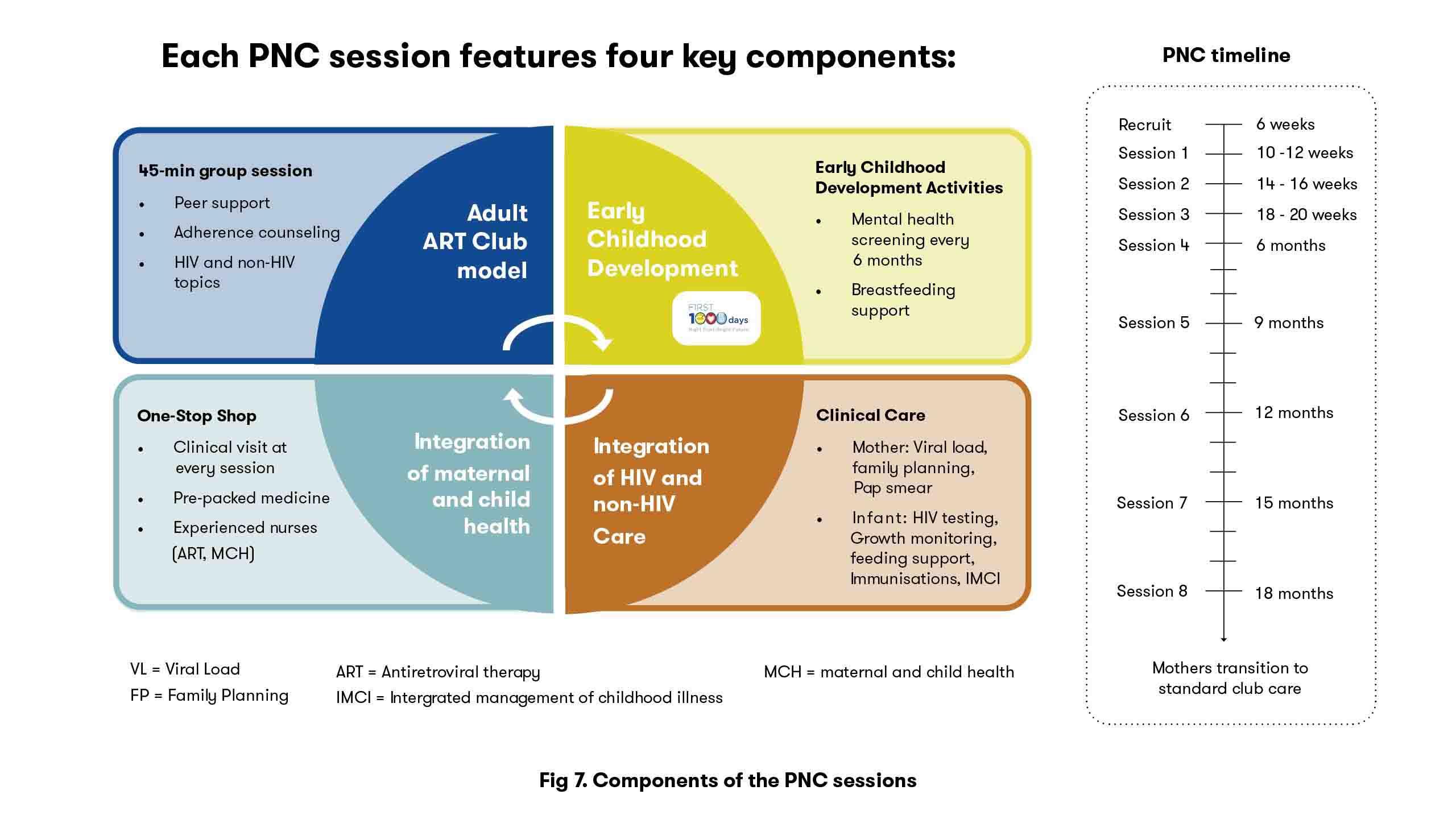
6. Group session
The mothers and babies start by sitting in a circle and the PNC facilitator then facilitates a health education and ECD activities session as per the guide below.
Full session guides are found here.
The PNC facilitator will weigh the mother and baby. Mothers are asked about symptoms of TB at every visit and screened for depression every 6 months. The facilitators complete a depression screening form to identify mothers at risk. This is then reviewed by the nurse at the clinical visit. The Perinatal Mental Health Project (PMHP) provides instruction on mental illness and psychosocial risk screening in postnatal women.
Download the PMHP maternal risk screening tool and see the link to the PMHP website here.
The babies are screened for general illness. If the baby shows signs of acute severe illness, they are fast-tracked to see the nurse. Everything is recorded into the club register by the PNC facilitator.
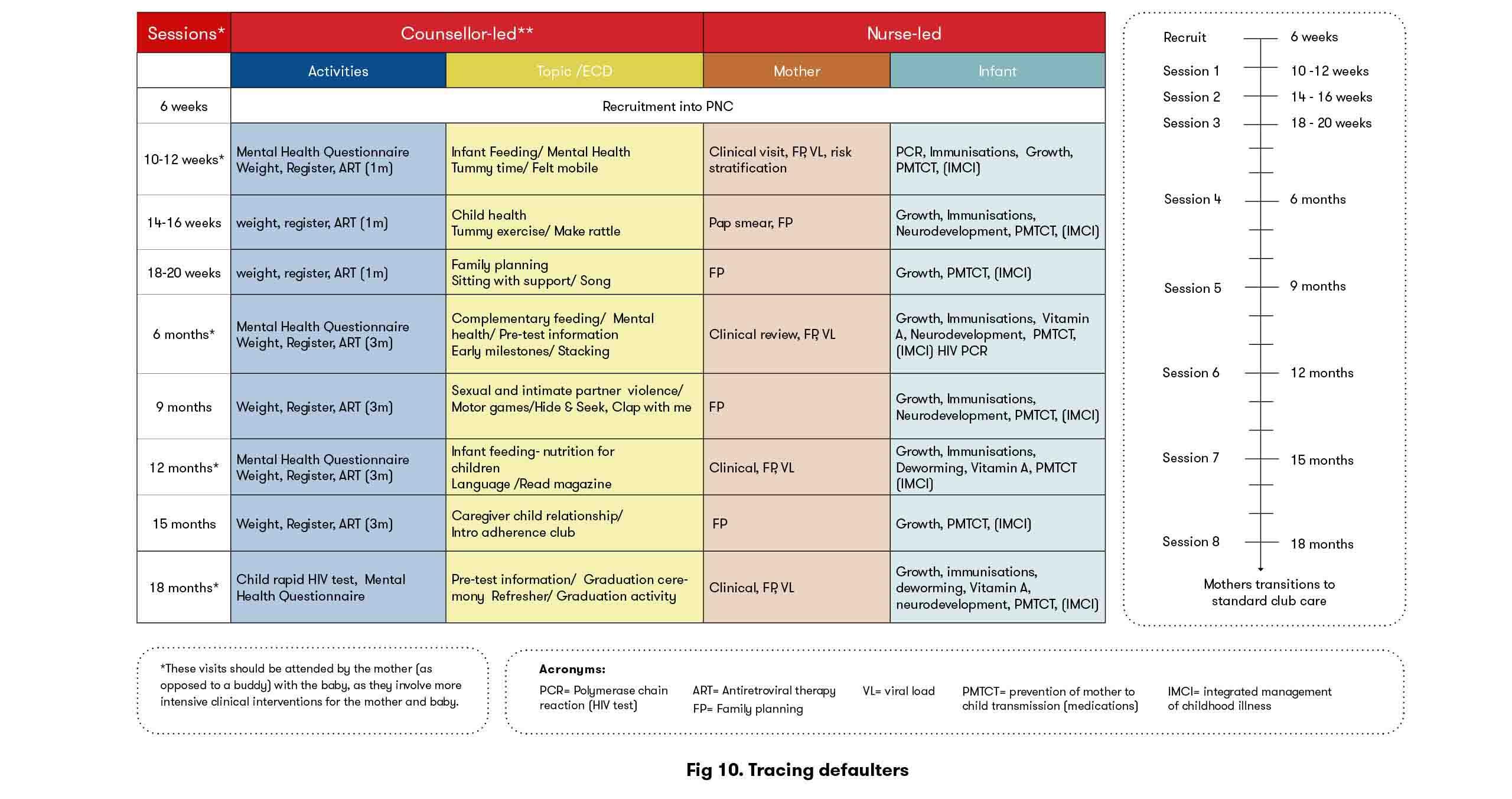
Each session includes information on adherence, infant feeding (encouraging exclusive breastfeeding) and health promotion messages which change at each visit—some messages are HIV-related topics whilst others are not. Some topics covered include HIV status disclosure, sexual violence, family planning and education on VL suppression.
Each session ends with education about ECD. The PNC facilitator talks about developmental milestones and shows the mothers how to do some ECD activities. Mothers and PNC staff are encouraged to bring recyclable material to the sessions to do the ECD activities.
Whilst the MIPs wait to see the nurse, the PNC facilitator distributes the ART (pre-packed for one month or three months depending on the club) to the mother and they inform them of their next appointment date. The mothers also receive a schedule of all the PNC visits at the first visit
High-risk mothers* receive extra psychosocial support. Even when the clubs are three-monthly, high-risk mothers are seen monthly.

7. Clinical visit: one-stop-shop for mother-infant pairs


The nurse will encourage breastfeeding and evaluate the PMTCT needs of the baby according to their age. This includes HIV testing and various prophylactic medicines, including Nevirapine, AZT, and Cotrimoxazole syrups.


The mother has a full clinical visit at the baseline visit (10 weeks), at the 6-month visit and then 6-monthly. The clinical visit includes a review of the mother’s HIV care and VL testing. It also includes being screened for hypertension, cervical cancer (Pap smear), and depression. The mother is referred to the PNC doctor if screening positive for depression, hypertension or if any other health problem is encountered that needs medication other than ART.
At each PNC, the mother will be assessed for her need for family planning that day. Long-acting methods, such as the intra-uterine contraceptive device (IUCD) are promoted.


If the mother is high-risk, she is seen monthly by the nurse (outside the club if clubs are three-monthly) and only given a one-month supply of medication. The nurse also provides enhanced adherence support (in Western Cape, we use the risk of treatment failure program).
Extra observations are performed by the PNC nurse as needed, during the club clinical visit, saving further time as queues are avoided. Patients should be managed as per local guidelines, see NDoH PMTCT Guidelines.
8. Post-PNC follow-up
msf.localAfter the club, a number of follow-up actions are taken by the PNC facilitators.
In the week after the PNC, the PNC facilitators check the results of the mothers’ VL tests and the infant PCR tests. They place results into the respective mother and infant folders. If maternal VL>50 copies/ml or the baby’s PCR is positive, the PNC facilitator immediately informs the nurse. The nurse will then recall the mother and her baby to be seen as soon as possible.
9. Tracing of mother-infant pairs
Mothers should attend club sessions that include scheduled VL testing, but may send a buddy with the baby in her stead on other visits. If the mother (or buddy) and baby do not attend a PNC session, the PNC facilitator is responsible for recalling the mother within 2-3 days. If the mother has not presented by Day 5, an PNC facilitator or CCW will carry out a home visit. If the patient does not present to care within 2 weeks of the home visit, she is considered as a defaulter and would be recorded as such in the register. She would however be accepted back into the PNC if she comes back at a later stage. This is a major difference from a normal adult ART club, in an effort to retain the high-risk mothers in PNC care.

monitoring-and-evaluation
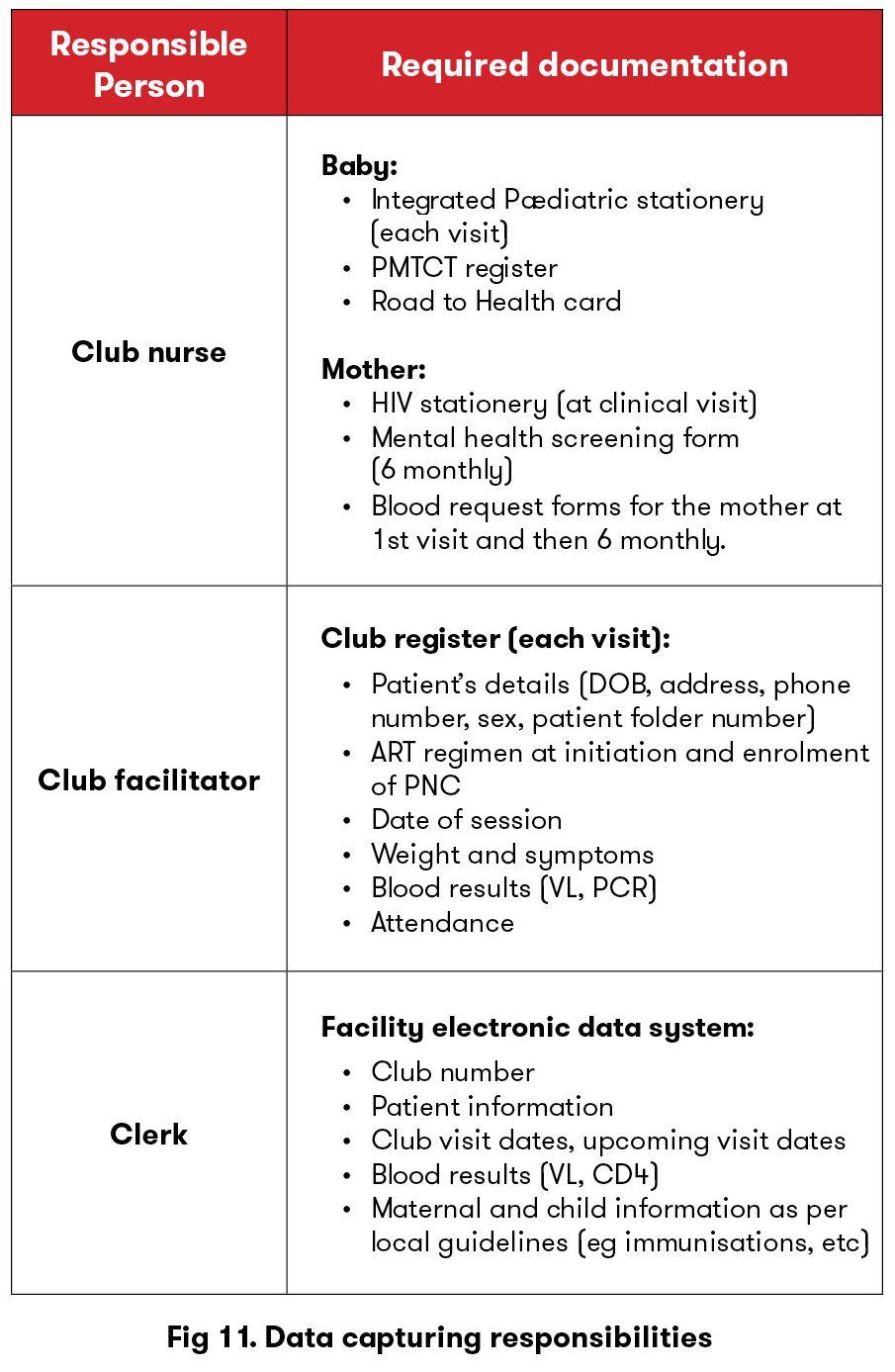
The PNC facilitator records PNC data into the club register. The club nurse completes the integrated paediatric stationery, which encourages integrated care and prompts the nurse as to which services should be rendered at each visit. The nurse fills in the paediatric stationery in the baby’s folder at each visit, but she only writes in the mother’s folder at the mother’s clinical visits or if she receives family planning. For all other visits, the mother’s information is recorded in the club register.
- City of Cape Town Paediatric Stationery (July 2017)
- ART register Club Register (August 2016)
2. Data capturing
Data clerks should ensure that all the latest blood results of the mothers are filed in the folder.
Facility clerks regularly capture the PNC visits into an electronic data system, using a combination of the club register and the mothers’ and babies’ folders for other services rendered. The mothers’ and babies’ folders are kept together in crates, per PNC number, at the reception, where all folders are kept. This is clearly identified on the mothers’ and babies’ cards so that their folders are easily retrievable in case they come for a clinical visit outside the PNC.
Once the data capturing is completed, the clerk has to sign off each page that has been captured. When all patients’ information has been transferred into the electronic system, the cover page of the club register will be signed off.
A summary of who is filling in and capturing what is provided in the table below.
Quantitative Results
From June 2016 to 31st December 2018, we recruited 433 mothers (27 high-risk) and 439 infants (6 sets of twins).
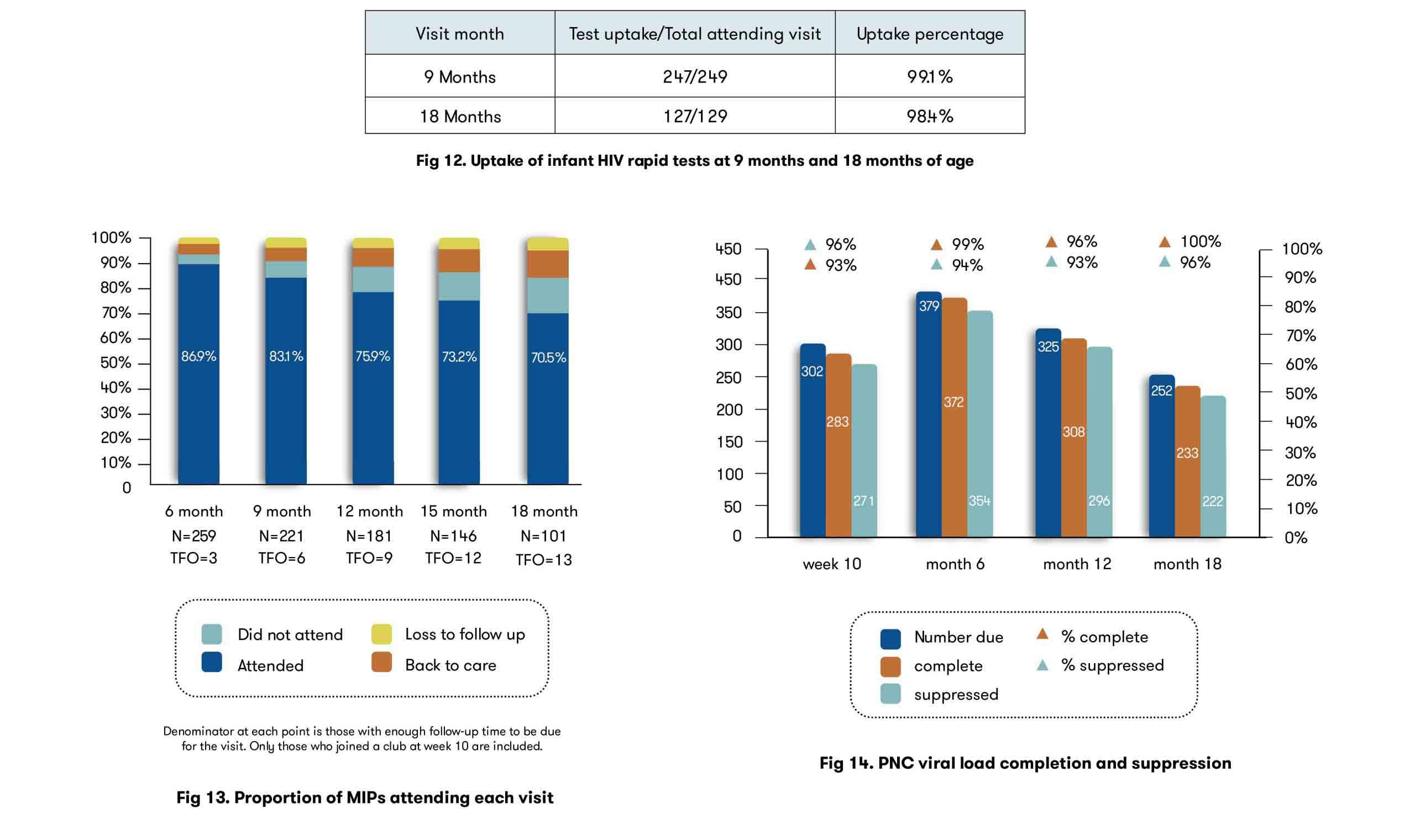
Uptake of infant HIV testing was high at age 9 months (99.1%) and 18 months (98.4%). No seroconversions of infants were observed (See Figure 12).
Of those reaching their 18-months visit, 70.5% of pairs were still in care (see Figure 13).
Of the 141 mothers who were eligible for a pap smear, 53.2% received a pap smear by 18 months.
Of all the women who had a mental health screening, 17.5% screened positive for depression on at least one occasion.
Maternal viral load testing and suppression remained above 90% throughout PNC (see Figure 14).
Out of a total of 187 confirmed infants’ vaccination coverage at 12 months, 88.9% were fully immunised.
** Protocol was approved by Foundation Professional Development-Ethics Research Board and by MSF-ERB
Time and Motion Study
Challenge: length of club visit
The peer support group session is lengthy at 30 to 45 minutes, and a dedicated counsellor or peer mentor is required to facilitate the session. In addition, the PNC nurse and clinic management initially felt that the clinical visit was very lengthy and that too many services were being rendered at the PNC. They suggested that some interventions (i.e. Pap smear) should be shifted back to other clinic staff.
An informal “time and motion study” challenged this perception, showing that the time taken to provide all PNC services in a non-integrated way differed little from the duration of an integrated PNC clinical visit. Following further discussions, staff unanimously agreed that no services should be removed from the PNC model.
Challenge: meeting headcount targets
In the City of Cape Town health system, nurses have a target number of patients to see per day (“headcount”). Initially, there was concern that the PNC nurse was not seeing enough patients.
This headcount does not take into consideration that multiple services are being offered. Such targets should be changed to the number of services rendered to more accurately reflect the workload. It is also important to note that an integrated clinical visit provides an improved quality of care, as seen in an audit of the City of Cape Town PMTCT –PNC indicators.

Qualitative Study
We conducted a qualitative study in September 2017 to look at “Knowledge transmission, peer support, health-seeking behaviour and satisfaction in Postnatal Clubs in Khayelitsha, South Africa”. 10 IDIs (individual interviews), 3 FGDs (focused group discussion) and 2 POs (observations) were conducted with PNC participants, staff and key informants in isiXhosa and English until reaching saturation. Findings of the study are below and were published ****
*** Protocol was approved by University of Cape Town Ethics Board, ITM IRB, UZA/UA and MSF ERB
****Knowledge transmission, peer support, behaviour change and satisfaction in Post-Natal clubs in Khayelitsha, South Africa: a qualitative study
"Before a child is tested, you receive counselling. All of us we would talk about the test that is going to be done on the baby"PNC participant

Tools
Click to download:
PNC Scheduler
PNC session guide
ROTF worksheet
Club Register
Standard operating Procedure on Postnatal clubs
Road to Health Booklet
City of Cape Town Paediatric Stationery
Post Natal Clubs Review of model
PMHP maternal Risk Screening Tool
Job Description Club Facilitator
Job Description Checklist Data Clerk
Job Description Checklist PNC Nurse
Job responsibility Checklist Pharmacy Assistance
PNC Training Manual
Facilitators attend 3 days of training, nurses attend the last 2 days of training, facility managers/OPM/Clerk/pharmacy assistant/doctor attend the last day of training.
Conclusions
Through the PNC model, we were able to improve maternal retention in HIV care and postpartum Viral Load completion and suppression. We were also able to realize a higher uptake of infant HIV testing until 18 months of age, and experienced no infant seroconversions.
A qualitative study also showed high levels of satisfaction among participating mothers. The PNC model allows for the comprehensive integration of a number of healthcare services for the mother-infant pair. Given the high uptake of several services and favourable outcomes through the PNC model, PNCs are being scaled up in other clinics in South Africa. This model can also be adapted with relative ease to be implemented in or other resource-limited settings with substantial burdens of HIV.


Acknowledgements
Shariefa Abrahams, Kornelia Flami, Leila Stein, Orli Setton and Shaun Brassell.
All of existing and previous MSF team members (Tabitha Mutseyekwa, Leticia Mdani, Nompumulelo Mantangana, Aurelie Nelson, Leigh Snyman, Damian Hacking, Tali Cassidy, Keitu Lebelo, Nikiwe Malabi, Laura Trivino Duran, Rodd Gerstenhaber, Kate Buchanan, Julia Hill, Catherine Wedderburn, Marianna Garcia, Rinako Uenishi, Esther Casas, Sean Christie, Suhair Solomon, Simone Honickman, Lynne Wilkinson, Paola Lopez, Vinayak Bhardwaj and Bulelwa Rorwana).
Mothers2mothers staff and their support team provided astounding care and listening skills to all the mothers.
COCT and Town 2 staff were instrumental in supporting the intervention from the start and help remodel it as we piloted it.
All photos by Leila Stein and Sean Christie/MSF
Acronyms
ART - Antiretroviral therapy
ARV - Antiretroviral
CDU - Central dispensing unit
CF - Club facilitator
CN - Club nurse
ECD - Early childhood development
FM - Facility manager
FP - Family planning
HR - Human resource
IMCI - Integrated management of childhood illness
IUCD - Intrauterine contraceptive device
M2m - Mother 2 mothers
MIP - Mother-infant pair
MSF - Médecins Sans Frontières
MTCT - Mother to child transmission
PCR - Polymerase chain reaction
PMHP - Perinatal Mental Health Project
PMTCT - Prevention of mother to child transmission
SOP - Standard operating procedure
RIC - Retention in care
ROTF - Risk of treatment failure
VL - Viral load
References
- UNAIDS. 2015 Progress report on the global plan towards the elimination of new HIV infections among children and keeping their mothers alive [Internet]. Vol. 11, Unaids. 2015. p. 1–88. Available here
- Ramraj T, Goga AE, Larsen A, Ramokolo V, Bhardwaj S, Chirinda W, et al. Completeness of patient-held records: observations of the Road-to-Health Booklet from two national facility-based surveys at 6 weeks postpartum, South Africa. J Glob Health [Internet]. 2018;8(2):1–13. Available here
- Clouse K, Schwartz S, Rie A Van, Bassett J, Yende N, Pettifor A. " What They Wanted Was to Give Birth; Nothing Else " : Barriers to Retention in Option B+ HIV Care Among Postpartum Women in South Africa. J Acquir Immune Defic Syndr. 2014;67(1):12–8.
- Phillips T, Thebus E, Bekker L-G, Mcintyre J, Abrams EJ, Myer L. Disengagement of HIV-positive pregnant and postpartum women from antiretroviral therapy services: a cohort study. J Int AIDS Soc [Internet]. 2014;17:19242
- Suthar AB, Hoos D, Beqiri A, Lorenz-Dehne K, McClure C, Duncombe C. Integrating antiretroviral therapy into antenatal care and maternal and child health settings: a systematic review and meta-analysis. Bull World Health Organ [Internet]. 2013;91(1):46–56. Available here
- Hodgson I, Plummer ML, Konopka SN, Colvin CJ, Jonas E, Albertini J, et al. A systematic review of individual and contextual factors affecting ART initiation, adherence, and retention for HIV-infected pregnant and postpartum women. PLoS One. 2014;9(11).
- Nachega JB, Hislop M, Dowdy DW, Lo M, Omer SB, Regensberg L, et al. Adherence to Highly Active Antiretroviral Therapy Assessed by Pharmacy Claims Predicts Survival in HIV-Infected South African Adults. JAIDS J Acquir Immune Defic Syndr [Internet]. 2006;43(1):78–84.
- Nachega JB, Uthman OA, Anderson J, Peltzer K, Wampold S, Cotton MF, et al. Adherence to antiretroviral therapy during and after pregnancy in low-income, middle-income, and high-income countries. AIDS [Internet]. 2012 Oct;26(16):2039–52. Available here
- Christina Psaros, Jocelyn E. Remmert, David R. Bangsberg SAS, Smit and JA. Saharan Africa : Falling Off the Cliff of the Treatment Cascade. Curr HIV/AIDS Rep. 2016;12(1):1–5.
- Project UA. Mother-To-Child Transmission of HIV Interventions With Maternal , Newborn , and Child Health Services. Integr Vlsi J. 2011;1(February):1–19.
- Luque-Fernandez MA, Van Cutsem G, Goemaere E, Hilderbrand K, Schomaker M, Mantangana N, et al. Effectiveness of Patient Adherence Groups as a Model of Care for Stable Patients on Antiretroviral Therapy in Khayelitsha, Cape Town, South Africa. Dowdy DW, editor. PLoS One [Internet]. 2013 Feb 13;8(2):e56088. Available here
- Grimsrud A, Sharp J, Kalombo C, Bekker L-G, Myer L. Implementation of community-based adherence clubs for stable antiretroviral therapy patients in Cape Town, South Africa. J Int AIDS Soc [Internet]. 2015 Jan 27;18(1):19984. Available here



